COVID19_multi-language
1.Common history of new coronavirus infection (COVID-19) (Japan Primary Care Association)
- The patients develop cold-like symptoms (fever, cough, sputum, sore throat, runny nose, etc.) and have strong fatigue, after an incubation period of about 5 days (1-14 days),
- Some patients may have gastrointestinal symptoms such as vomiting and diarrhea,
- The symptoms are last for about 7 days,
- 80% of patients are mild and recover spontaneously, 20% of patients have severe pneumonia, and hospitalization is required, 5% of patients may require intensive care and respiratory treatment,
- In particular, senior citizens, people with underlying health conditions and pregnant women may develop pneumonia immediately after onset,
- Beware that if the disease becomes severe, it will quickly worsen and may lead to death.
* It is difficult to diagnose only with the symptoms because the symptoms are similar to flu and cold.
2.If you feel concerned about COVID-19
- If you have a fever of 37.5 degrees or higher, stay home and refrain from immediately consulting medical consultation.
- Avoid going out unnecessary.
- If you (general population) feel strong fatigue, difficulty in breathing, or have no urine, consult with Call Centers for Japanese Returnees and Potential Contacts at each prefecture. If the consultation center suspects that you have been infected with the virus, it will introduce you to an available medical institution with COVID-19 testing ad treatment.
- The contact numbers in each prefecture are listed in the URL below. https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/kenkou_iryou/covid19-kikokusyasessyokusya.html
- Senior citizens, persons with underlying health conditions, and pregnant women have symptoms for two days, consult with Call Centers for Japanese Returnees and Potential Contacts at each prefecture.
- If your symptoms persist for four days, consult with the Call Centers for Japanese Returnees and Potential Contacts at each prefecture.
- You may refer to the Tokyo metropolitan COVID-19 website in the URL below.
https://stopcovid19.metro.tokyo.lg.jp/en/flow
3.Testing of COVID-19
- The diagnosis test is PCR (a method of detecting and increasing the amount of virus). PCR screening is now covered by health care insurance to facilitate the necessary tests for patients. Call Centers for Japanese Returnees and Potential Contacts (available 24 hours) suggest necessary to conduct screening. The patients become eligible to request a test directly from one of the private-sector screening institutions without going through a public health center.
- If the result is positive, almost 99% can be said to be an infected with Novel coronavirus as a definitive diagnosis. If it is negative, 30-70% of people do not mean that he/she is not infected. Thus, if symptoms persist, a repeated test is needed.
4.Reasons for the spread of new coronavirus infections
- The virus can spread from person to person through small droplets from the nose or mouth, which are spread when a person with COVID-19 coughs or exhales. These droplets land on objects and surfaces around the person. Other people then catch COVID-19 by touching these objects or surfaces, then touching their eyes, nose, or mouth. People can also catch COVID-19 if they breathe in droplets from a person with COVID-19 who coughs out or exhales droplets.
- Some spread might be possible before people show symptoms.
- 10-20 % of people with COVID-19 experience no symptoms at all and many people experience only mild symptoms. This is particularly true in the early stages of the disease. It is, therefore, possible to catch COVID-19 from someone who has, for example, just a mild cough and does not feel ill.
- If you are healthy, you only need to wear a mask if you are taking care of a person with suspected COVID-19 infection. Wear a mask if you are coughing or sneezing. Masks are effective only when used in combination with frequent hand-cleaning with alcohol-based hand rub or soap and water.
- If you wear a mask, then you must know how to use it and dispose of it properly. <
- Normal masks are less effective because viruses can pass through.
5.To prevent COVID-19 infection
Refrain from activities in the places where the following three conditions were met simultaneously:
- Closed space with poor ventilation,
- Crowded with many people and
- Conversations and vocalization in close proximity (within arm's reach of one another)
Reference:
1. https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/newpage_00032.html
https://www.mhlw.go.jp/content/10900000/000607599.pdf
2. https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/kenkou_iryou/dengue_fever_qa_00014.html#Q2
3. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/how-covid-spreads.html
https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public
https://www.who.int/news-room/q-a-detail/q-a-coronaviruses
4. https://www.mhlw.go.jp/content/10900000/000611515.pdf
Written by Nakasa and Koto
*****
1.Global and Japanese Situation of COVID-19
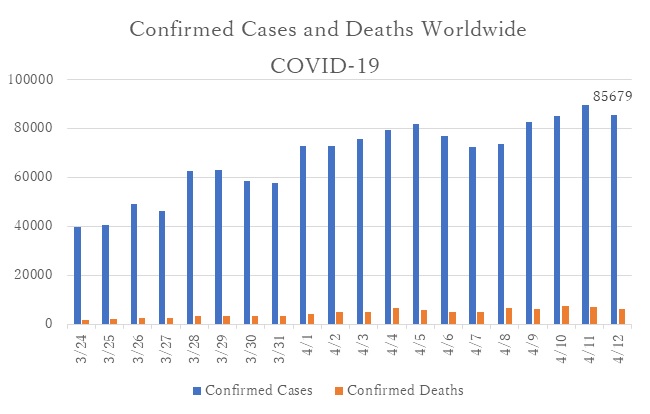
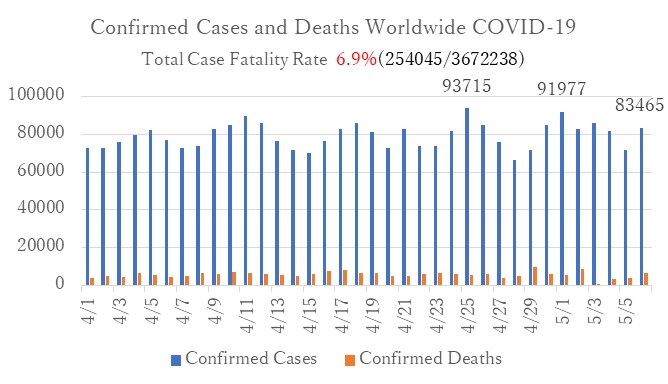
Number of the new confirmed Case
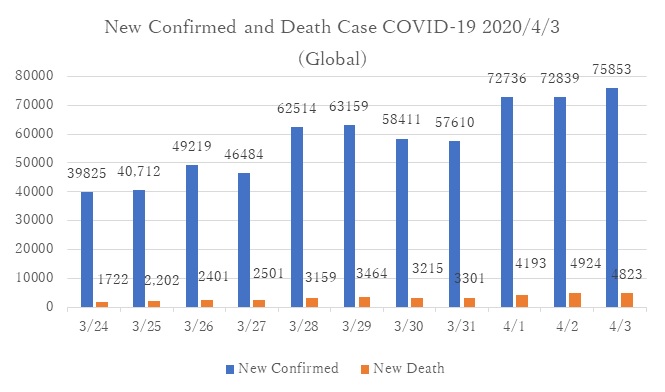
■WHO Coronavirus disease 2019 (COVID-19) Situation Report 2020/4/3
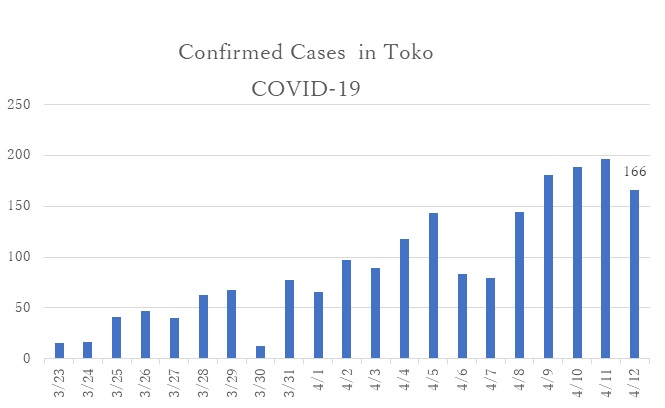
■Tokyo 2020/04/04: Tokyo Prefecture Report
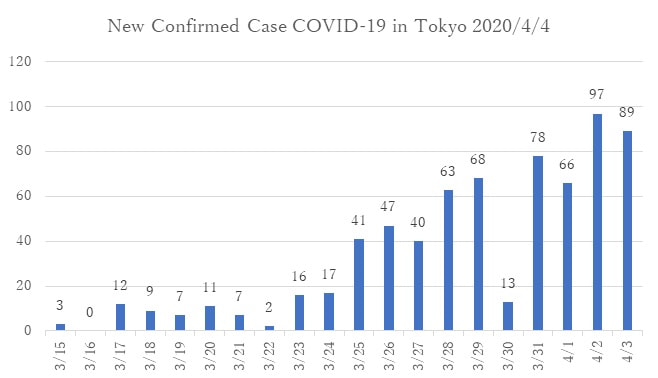
•The number of new confirmed cases is gradually increasing. Clusters at health felicities have been confirmed. Health officials concerned the explosive outbreak.
2.Clinical conditions of the Coronavirus disease (COVID-19): Why the COVID-19 patients become critically ill and die in a short period?
While most people with COVID-19 develop only mild or uncomplicated illness, approximately 14% develop severe disease (WHO, 2020). Mr. Ken Shimura, well known Japanese comedian, had severe pneumonia at four days of onset. Although he received mechanical ventilation and extracorporeal membrane oxygenation at the Intensive Care Unit (ICU), he lost consciousness and deceased.
The case report from Seattle, USA (Bhatraju et al., 2020), and Wuhan, China (Guan et al., 2020)
- • Senior citizens and people with chronic medical conditions (e.g., diabetes mellitus, chronic kidney diseases, and asthma) were common in the critically ill population.
- • COVID-19 patients become a critically ill in a short period. Of the 24 patients, 12 patients have died on average of 7.5 days at the ICU in Seattle. Patients had respiratory failure leading to hypotension (i.e., low blood pressure). /li>
- • COVID-19 can be complicated by the acute respiratory distress syndrome (ARDS), sepsis and septic shock, multiorgan failure, including acute kidney injury and cardiac injury (WHO, 2020).
- • Among the COVID-19 patients, lymphocytopenia (an abnormally small number of lymphocytes) was common in both cases in Seattle and Wuhan. It may cause acute immune deficiency.
3.Mechanical ventilation and extracorporeal membrane oxygenation (ECMO)
Gas exchange is the delivery of oxygen from the lungs to the bloodstream, and the elimination of carbon dioxide from the bloodstream to the lungs.
- Mechanical ventilation is also called a ventilator, respirator, or breathing machine. The ventilator pushes a mixture of air and oxygen into the patient's lungs to get oxygen into the body.
- Extracorporeal membrane oxygenation (ECMO) is a treatment uses a pump to circulate blood through an artificial lung back into the bloodstream. Acute respiratory distress syndrome causes cardiac injury. Therefore, patient in critical conditions needs the life-support with ECMO. These advanced medical therapies require extensive trainings for medical professionals (i.e., physician, nurses, biomedical medical equipment technician, etc.). Therefore, it is a matter of not only preparing medical equipment but also human resources.
4.Myth about COVID-19(WHO)
※The following information has no foundation
- Exposing yourself to the sun or to temperatures higher than 25C degrees to prevent the coronavirus diseases (COVID-19).
- Although recovering from COVID-19, you will have the COVID-19 virus in the body for the life.
- Holding the breadth for 10 seconds or without coughing or feeling discomfort, you are free from the COVID-19.
- Drinking alcohol protect you against COVID-19.
- COVID-19 virus can be transmitted in hot and humid weather.
- Cold weather and snow kill the COVID-19 virus.
- Taking a hot bath prevent the COVID-19.
- COVID-19 can be transmitted by through mosquito bites.
- Hand dryers are effective in killing the COVID-19 virus.
- Ultraviolet disinfection lamp (UV lamp) kill the COVID-19 virus.
- Spraying alcohol or chlorine all over your body kill the COVID-19 virus.
- Rinsing your nose with saline help prevent infection with the COVID-19 virus.
- Eating garlic help prevent infection with the COVID-19 virus.
- Antibiotics are effective in preventing and treating the COVID-19.
Reference:
1.Covid-19 in Critically Ill Patients in the Seattle Region -- Case Series
https://www.nejm.org/doi/full/10.1056/NEJMoa2004500?query=featured_coronavirus
2.Clinical characteristics of 2019 novel coronavirus infection in China
https://www.medrxiv.org/content/10.1101/2020.02.06.20020974v1
3.Clinical management of severe acute respiratory infection(SARI) when COVID-19 disease is suspected
https://www.who.int/docs/default-source/coronaviruse/clinical-management-of-novel-cov.pdf
4.COVID-19 is an emerging, rapidly evolving situation
https://medlineplus.gov/ency/anatomyvideos/000059.htm
https://medlineplus.gov/ency/article/007234.htm
5.American Thoracic Society
https://www.thoracic.org/patients/patient-resources/resources/mechanical-ventilation.pdf
6. Coronavirus disease (COVID-19) advice for the public: Myth busters (WHO)
https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/myth-busters
*****
1.Global and Japanese Situation of COVID-19
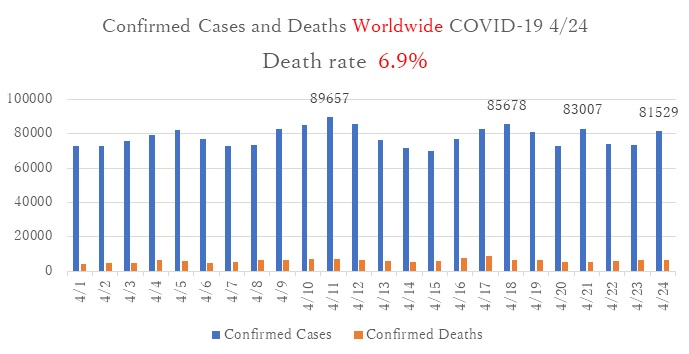
Confirmed cases of COVID-19 worldwide according to reports by WHO Update 2020/4/12(Japan Standard Time)
2.Measures being implemented by the Japanese Government (Ministry of Health, Labour and Welfare) against the spread of COVID-19
- In cases where new COVID-19 are confirmed, the official policy is to investigate the existence of asymptomatic close contacts [1], isolate them and monitor their health for signs of COVID-19.
- Investigating asymptomatic close contacts among cluster cases, isolate, and monitor.
- Promoting good hygiene practices as means of raising public awareness about the prevention of the spread of COVID-19 using media campaigns.
- Treating the patients with symptoms of COVID-19 at medical facilities, provide intensive care (e.g., mechanical ventilation and extracorporeal membrane oxygenation) for severe patients.
- Patients with mild symptoms are transferred from hospitals to other facilities such as hotels where they are operated by medical staff, and thereby reduce the load on medical staff on the frontline of medical care.
[1]
According to the MHLW, the "close contact with infected persons" generally mean as follows:
- Touching an infected person directly, without anti-infective measures
- Meeting an infected person at a distance of around 2 meters (6 feet) or less
https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/kenkou_iryou/dengue_fever_qa_00014.html#Q7
3.What to do at home
It is very important to initiate good hygiene practices at home.
Guidelines of washing hands at home are followed:
- After returning home from outside
- After touching things (such as doorknobs) that other people may have touched
- After coughing, sneezing, or blowing your nose
- After taking care of a person with symptoms
- Before cooking and eating
- After handling human or animal excrement
- After using the toilet
Guidelines of cleaning house and reducing possibility of infections are followed:
- Wear disposable gloves to clean rooms.
- Clean all surfaces that are touched often every day, like doorknobs, light switches, countertops, desk, remote-control, phones, handles, toilets, faucets, and sinks.
- Wash laundry thoroughly, including cushion and sofa cover.
- Open windows for ventilation (5 to 10 minutes, every 1 to 2 hours during daytime)
Guidelines of taking care of family members are followed:
Use a separate bedroom and bathroom for a person who is sick (if possible) and open a window for ventilation.
- Wash your hands often with soap and water for at least 20 seconds, especially after interacting with the sick person.
- Wear masks (patients and family members) when you contact within 1-2 meters.
- Ensure that the same person takes care of the sick person (if possible). Wear disposal gloves, and masks. Dispose them in separate bags, and wash hands every time after contacts.
- Avoid touching your eyes, nose, and mouth with unwashed hands.
- Do not share plates with other family members. In case it is necessary to share with other family members, soak in disinfectant or boiled water for 10 minutes before washing with detergents.
- Do not share clothes and bed linens as they be contaminated with body fluids (e.g., vomits, diarrhea). Soak in 80℃ water for 10 minutes, wash separately from other family members. The most common household bleach will work[2].
[2]
0.1% for cleaning of body fluids (e.g., vomits, diarrhea): two caps of pet bottle (10ml) in 500ml water
0.05% for regular cleaning (e.g., kitchen stainless, doorknobs, toilet, floors): one caps of pet bottle (5ml) in 500ml water
4.Triage of severe patients
- Triage is a term utilized in emergency and disaster. It the process of sorting victims, as of disaster such as earthquake, to determine medical priority in order to increase the number of survivors.
- Explosive outbreaks of COVID-19 will result in an overwhelming the capacity of medical facilities to handle infected people not only in terms of medical equipment but also human resources. Triage to sort severe and mild cases might be necessary. For example, a patient who is likely to survive and live is more likely to be supported by ventilators and other life-saving equipment. In contrast, others who are unlikely to respond to treatments would not be supported. There have been reports of such cases in other countries. Our organization hopes that this does not arise in Japan.
Reference:
1.https://www.mhlw.go.jp/content/10900000/000620733.pdf
2.https://www.cdc.gov/coronavirus/2019-ncov/if-you-are-sick/index.html
3.http://www.tohoku-icnet.ac/Control/activity/images/guide/post_200316.pdf
4.https://www.nytimes.com/2020/03/21/us/coronavirus-medical-rationing.html
Koto K, RN, SHARE advisor
*****
1.Global and Japanese Situation of COVID-19
Confirmed cases of COVID-19 worldwide according to reports by WHO Update 2020/4/12 (Japan Standard Time) : Ministry of Health, Labor and Welfare (MHLW)
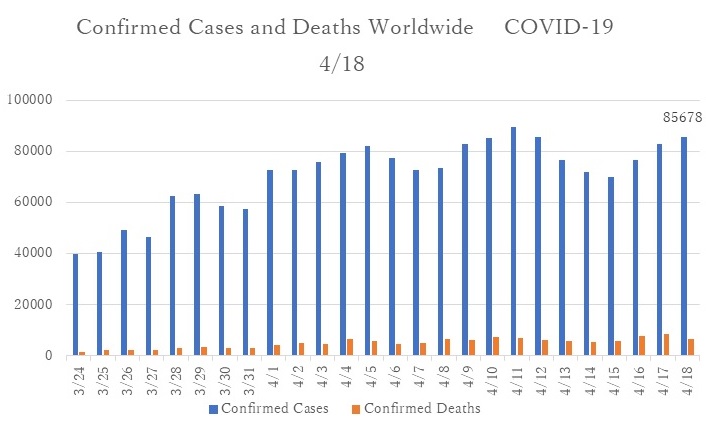
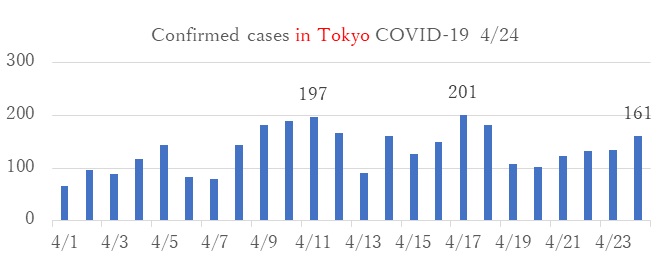
Tokyo 2020/4/18 (Japan Standard Time): Tokyo Prefecture Report
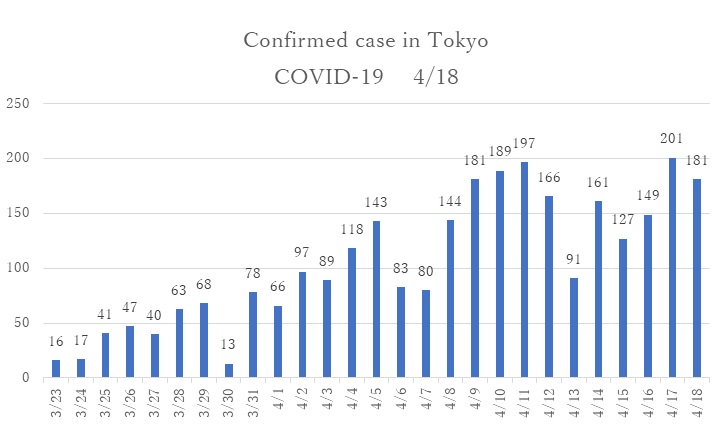
- The number of confirmed cases continues to exceed 100 cases per day after the Japanese government declared the state of emergency on 7 April.
- On April 16, the Japanese government declared the national state of emergency to prevent further spread of COVID-19 virus from high populated prefectures to other areas.
2.First「National survey on COVID-19」on 31 March to 1 April, 2020
- The joint survey was conducted collaboration of MHLW and LINE Corporation. 24 million of Japanese residents (approximately 20 percent of total population) participated in this survey. The survey was an innovative survey method that enabled to collect data in limited time with low-cost. However, because the targeted population was people who used LINE in daily life, this survey methods showed some limitations: People with severe symptoms had low respond rates due to difficulty of engaging in LINE; People with high health literacy of infection prevention more likely to present the high respond rates.
- The questionnaire consisted of age, zip-code, gender, and health condition (normal, fever more than 37.5 ℃, sore throat, strong fatigue, cough, other not feeling well).
- The participants were categorized into six groups: (1) People who were in the service industry and could not avoid the three Cs[1](e.g., food services, salespeople that involve face-to-face contacts); (2)People who obtained knowledge of the infection prevention (e.g., health professionals, long-term care specialists); (3) People who were involved in works where already implemented measures to avoid three Cs (e.g., office work, retail industry, delivery services); (4) People who were involved in schools where temporarily closed as they followed measures to avoid three Cs (e.g., teachers, school staff, and students); (5) People who were able to practice social distance (e.g., housewives); and (6) People who did not belong to any of groups mentioned above.
(Result 1)
- The participants in Group (1) reported having a fever (more than 37.5 ℃ for four days) relatively higher than other groups (0.23% of total participants in Group (1)) in nationwide.
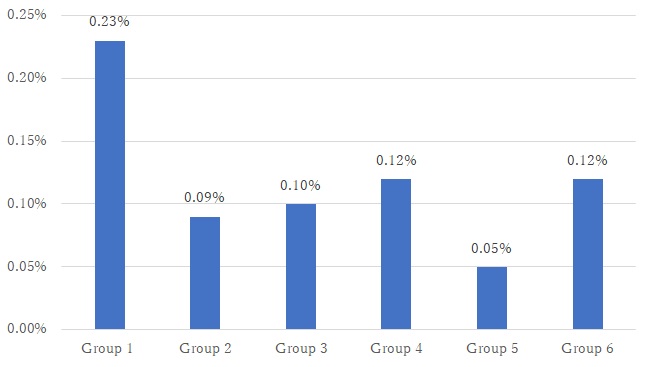
- Figure 1 The proportion of participants who reported having a fever
(Result2)
- The proportion of participants who reported having a fever was highest in Tokyo metropolitan(0.38%).
- (Recommendation: Required measures by the group)
- Participants in Group (5) reported having the least fever. From this result, it is considered that Group (5) may have been practicing social distances and measures to avoid the three Cs. This result showed that it is useful to prevent unnecessary outings to infect yourself or spread the infection to others.
- Group (1) could be the most vulnerable people to the risk of virus infection due to the nature of their working environments. It is urgently necessary to coordinate infection prevention measures to avoid the three Cs.
- The proportion of fever among Group (2) and Group (3) may correlatively increase as the infection risk increased in the community. It is necessary to maintain working environment with the measures to avoid the three Cs and to take social distance. Essential services (medicine, long-term care, retail industry, and delivery services) may require managing standard precautions under the critical circumstances.
- Group (4) is currently maintaining a social distance with the emergency school closures. Preparation of infection prevention practices is important for the resumption of school, such as face-to-face infection prevention education to avoid the 3 Cs, utilizing ICT for distance learning, and regular health checkups.
[1]
Closed spaces, Close proximity to others, and Close conversation
3.Was a new coronavirus infection epidemic predicted?(Emerging infectious Disease)
- COVID-19 and Ebola virus disease are emerging infectious diseases. According to WHO, the emerging infectious disease is defined as 'Newly recognized, newly evolved or occurred previously but have shown an increase in incidence or expansion of geographical, vector or host range'. Emerging infectious diseases have been under scrutiny since the 1990s, and they have become one of the most critical public health issues in the global health community, including avian flu, SARS, and MERS.
- A PUBLIC HEALTH EMERGENCY OF INTERNATIONAL CONCERN (PHEIC) is a formal declaration by the WHO as 'an extraordinary public health event which constitutes a public health risk to other States through the international spread of disease and may require a coordinated international response'. Under the 2005 International Health Regulations, countries have a legal duty to respond promptly to a PHEIC. Such events are required to be assessed for notification to WHO using a decision instrument. Four decision criteria used in the assessment of a public health event are (a) The seriousness of the event's public health impact. (b) The unusual or unexpected nature of the event. (c) The risk of international spread. (d) The risk that other countries will impose travel or trade restrictions. Any two criteria must notify to the WHO.
- A single case of smallpox, poliomyelitis (WPV), human influenza caused by a new subtype, and SARS must be immediately reported to WHO, irrespective of the context in which it occurs.
(Unexpected characteristics of COVID-19 infection)
- In global context, strategies, measures, and specific action plans have been prepared for emerging infectious diseases such as COVID-19 infections. However, the COVID-19 infection had unexpected impact due to the following reasons:
1:Typically, infectious disease spreads after patients become symptomatic. The new coronavirus has spread widely in asymptomatic cases.
2:Strategies and measures were prepared in the context of low- and middle- income countries where the health system is fragile, and to prevent pandemic to high-income countries. Explosive infections were not expected to prevail in high-income countries.
Referenceand further information:
1.https://www.mhlw.go.jp/stf/newpage_10798.html
2.https://www.japantimes.co.jp/news/2020/04/06/national/japan-social-distancing-talking-coronavirus/#.XpwZGy2KU0o
3.https://www.who.int/docs/default-source/documents/health-topics/standard-precautions-in-health-care.pdf?sfvrsn=7c453df0_2
4.https://www.who.int/ihr/procedures/pheic/en/
Koto K, RN, SHARE advisor
*****
1.Global and Japanese Situation of COVID-19
Confirmed cases of COVID-19 worldwide according to reports by WHO Update 2020/4/27 (Japan Standard Time) : Ministry of Health, Labor and Welfare (MHLW)
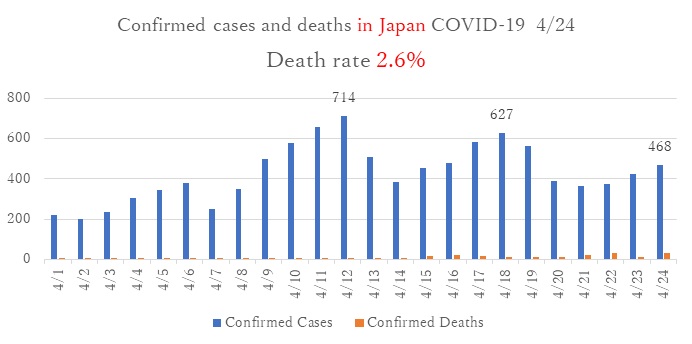
Tokyo 2020/4/24 (Japan Standard Time): Tokyo Prefecture Report
2.COVID-19 treatment for foreign residents in Japan
- Act on the Prevention of Infectious Diseases and Medical Care for Patients with Infectious Disease (The Infectious Diseases Control Law) was amended (Article 6. Item 8) to include COVID-19 as designated infectious disease.
- According to the Infectious Disease Control Law, the government covers the cost of COVID-19 medical treatments at hospitals and designated facilities. The patients may need to pay a maximum of 20,000 yen per month depending on household income.
- The cost of PCR testing is also covered, if it is ordered by the designated doctor (regardless of testing results).
- The cost of treatment before the isolation or without isolation will not be covered by government. Therefore, a patient with public health insurance need to pay 30% of the cost. If a patient without health insurance need to shoulder total amount of the cost.
- The Infectious Diseases Control Law covers all residents in Japan regardless of nationalities, resident's status, enlist in public health insurance.
Reference:
https://www.mhlw.go.jp/content/10900000/000589747.pdf
https://news.yahoo.co.jp/byline/kutsunasatoshi/20200127-00160618/
3.Management of the patients with mild cases
- Up until now, the confirmed cases have been treated at hospitals. Hospitals must keep available beds for severe cases as the number of confirmed cases is increasing. Therefore, the mild case patient will be transferred to the designated facilities.
- The mild case excludes (1) senior citizens, (2) persons with underlying health conditions (e.g., diabetes mellitus, cardiovascular disease, pulmonary disease, dialysis treatment), (3) persons with immunosuppressive (e.g., immune-suppressing drug, anticancer drug), and (4) pregnant women.
- • The mild case patients will be diagnosed by medical doctors of whether the patients will be hospitalized or who will send to medical facilities for PCR test. The doctors are also in charge of decisions of discharges from the designated facilities.
- The mild case patients will stay at the facilities designated by prefectural and city governments. The patients will stay until PCR test show negative twice continuously (this process takes approximately 14 days).
- The mild case patients are not allowed to leave the designated facilities. The cost of stay will be covered by the government, including meals. The patients might be charged for laundries (depends on the facilities).
- Nurses in charge of the designated facilities check patients' health condition regularly. In the case of worsening the health condition, the patients will be referred to hospitals.
Reference:
https://www.mhlw.go.jp/content/000625171.pdf
4.Border controls
- Measures against COVID-19 consist of prevention, diagnosis, isolation, and treatment. The border control is part of infection preventions to avoid further spread of infections by fever checking, interviewing, and providing necessary inspections to travelers.
- On March 18th, "New measures to tighten border controls were decided to take proactive measures aligning with measures taken by foreign countries.
- According to information on the risk of infection by MOFA[1] , travelers from countries above level 3 are subject of the border control. The travelers from countries on the list, the are asked to self-isolate at designated facilities by the quarantine station chief. All travelers must take PCR test, and the positive patients will be isolated and be monitored for fourteen days at hotels nearby the airports.
- Keio university hospital reported that among preoperative and prehospital patients, 6% positive asymptomatic patients were identified by PCR test. Although the test was conducted within one hospital, it infers that community-acquired infection in Tokyo metropolitan is about 6%. The actual infection rate among the population will be clarified by the proposed antibody test survey.
- The ongoing prevention strategies are combination of border controls to avoid new infection imported from outside of Japan, and infection preventions among residents in Japan through social distancing.
Reference:
https://news.yahoo.co.jp/byline/egawashoko/20200213-00162972/
- [1]The level (from 1 to 4) of the risk of infection are shown by the map in MOFA website.
Koto K, RN, SHARE advisor
*****
1.Global and Japanese Situation of COVID-19
Confirmed cases of COVID-19 worldwide according to reports by WHO Update 2020/5/7 (Japan Standard Time) :Ministry of Health, Labor and Wellfare (MHLW)
- Globally, the number of daily confirmed cases continues inreasing by more than 80,000.
- In Europe, while the number of daily confirmed cases decreased in Italy, France, and Germany within last month; Russia's daily confirmed cases is exceeding 10,000.
Tokyo 2020/5/07 (Japan Standard Time): Tokyo Prefecture Report
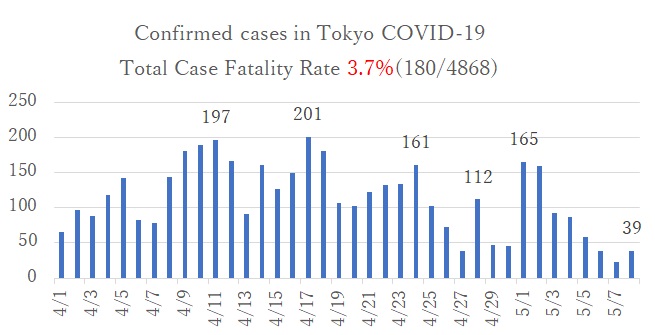
- The number of daily confirmed cases is decreasing nationwide as well as in the Tokyo metropolitan area. This might be an impact of staying home under the state of emergency. However, careful surveillance is necessary during these two weeks following Golden Week. Therefore, the Japanese government has extended the state of emergency until the end of the month.
2.Change definition of close contacts
- On April 20, MLHW changed definition of transmission period of COVID-19 from "the day of onset" to "2 days before the appearance of symptoms".
- The definition of close contacts includes these people as follows:
- Have lived together, or had long hours contact with the patients (e.g., in the train or aircraft).
- Have examined, nursed or cared for the patients without appropriate personal protective equipment.
- Have a high possibility of directly contacting airway secretions or body fluids of patients.
- Have been in contact with the patient for more than 15 minutes without any necessary infection prevention measures (mask, etc.) within a touchable distance (1 meter as a guide).
Reference:
https://www.niid.go.jp/niid/ja/diseases/ka/corona-virus/2019-ncov/2484-idsc/9357-2019-ncov-02.html
3.New coronavirus testing guidelines
- Up until now, the confirmed cases have been treated at hospitals. Hospitals must keep available beds for severe cases as the number of confirmed cases is increasing. Therefore, the mild case patient will be transferred to the designated facilities.
- On May 8, the MLHW eased access to the testing of COVID-19 infection.
- The new guidelines said that those who need to seek assistance immediately, and to call to a local health center, are as follows:
- Those who have one of symptoms such as difficulty in breathing, strong fatigue or high fever.
- Senior citizens, persons with underlying health conditions, and pregnant women who had mild cold symptoms.
- Those who have mild cold symptoms more than four days.
Reference:
https://www.mhlw.go.jp/content/000628620.pdf
4.Potential treatments and vaccines for the COVID-19
- Vaccination is one of the most effective ways to prevent disease. It helps the body's immune system to recognize pathogens like viruses, which keeps us safe from diseases. Therapeutic medicine is to treat after the symptoms appear, prevent worsen, and avoid death from the communicable disease.
- Human testing of investigational drugs consists of three phases.
- Phase1 to establish a drug's safety involving healthy volunteers,
- Phase 2 to assess the drug's effectiveness involving patient volunteers,
- Phase 3 to determine the effectiveness and identify other side effects by applying more number of patients
This process needs to be carried out ethically.
(Vaccine)
- WHO says 70 vaccines in the works, with three leading candidates as of April 13
- The furthest along in the clinical process is developed by Hong Kong-listed CanSino Biologics Inc. and the Beijing Institute of Biotechnology, which is in phase 2.
- The second is mRNA-1273 (RNA vaccine) developed by Moderna Inc and US National Institute of Health (NIH), which is in phase1.
- The third is INO-4800 (DNA vaccine) developed by Inovio Pharmaceutical Inc., which is in phase1. - Progress is occurring at with unprecedented speed in the development process, and the drug industry is hoping to compress the time to get a vaccine to market to within the next year.
(Therapeutic medicine)
- Currently, there is no therapeutic medicine which has been confirmed in its effectiveness scientifically to treat COVID-19. 109 clinical trials in the works, with leading candidates "Remdesivir" and "Favipiravir."
- Remdesivir was previously tested as an Ebola treatment. It has generated promising results in animal studies for MERS and SARS, which are also caused by coronaviruses, suggesting its effect in patients with COVID-19.
- Clinical trial in China reported on April 29 that there was no association of clinical benefits (e.g., faster time to clinical improvements) by utilizing Remdesivir (Wang, 2020).
- US NIH reported on the same date that Remdesivir accelerates time to recover and suggested decreasing mortality rate.
- On May 7, MLHW granted the Special Approval for Emergency on Remedisivir for the treatment of patients with COVID-19.
- Favipiraivir (Avigan), is a drug approved as an anti-influenza drug in Japan in 2014. It selectively and potentially inhibits the RNA polymerase (RdRp) of RNA viruses. It demonstrated anti-viral activity against Ebola virus (Furuta, 2017).
- Favipiravir is under clinical trials in Japan. However, the side effects on fetal anomaly limit its use on pregnant women and women expecting to become pregnant.
- Currently, there is no therapeutic medicine that has been shown to be safe and effective. Over 100 countries are working together to find effective therapeutics under solidarity clinical trial for COVID-19 launched by the WHO.
Reference:
・https://www.drugs.com/fda-approval-process.html
- Wang Y. et al., Remdesivir in adults with severe COVID-19: a randomized, double-blind, placebo-controlled, multicenter trial. Lancet, Published Online April 29, 2020.
・https://www.pmda.go.jp/english/int-activities/0004.pdf
- Furuta Y. et. al., Favipiravir (T-705), a broad spectrum inhibitor of viral RNA polymerase. Proc Jpn Acad ser B Phys Biol Sci. 2017; 93(7): 449-463.
Koto K, RN, SHARE advisor
*****
1.Global and Japanese Situation of COVID-19
Confirmed cases of COVID-19 worldwide according to reports by WHO Update 2020/5/14 (Japan Standard Time) :Ministry of Health, Labor and Wellfare (MHLW)
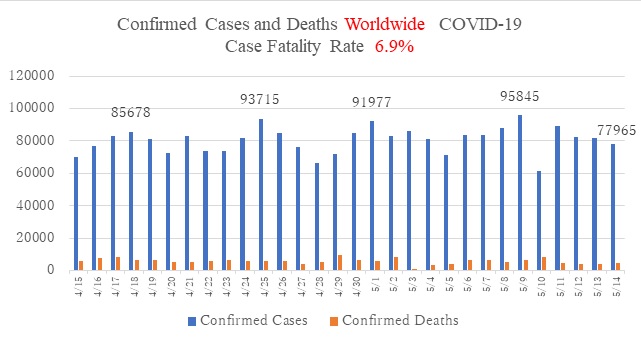
- Globally, the number of daily confirmed cases continues in the 70,000s.
- In Europe, while the number of daily confirmed cases decreased in Italy, France, and Germany within last month; UK's daily confirmed cases continue to remain consistently high, and Russia's daily confirmed cases keep exceeding 10,000. The governments around Europe have begun gradually easing lockdown restrictions. However, the fears of triggering a second wave of COVID-19 remains.
- In America, both the US and Canada, the number of daily confirmed cases continues to rise, although the rate of increase has lessened. In Brazil, Peru, and Chile, the rate of increase is growing and has reached a critical stage.
- In Asia (western pacific region, southeast Asian region), the rate of increase is slowing. No new confirmed cases have been reported in Laos, Vietnam, and Cambodia in the last two weeks. The number of daily confirmed cases in Indonesia and Singapore continues.
Tokyo 2020/5/15(Japan Standard Time): MOHLW, Japan
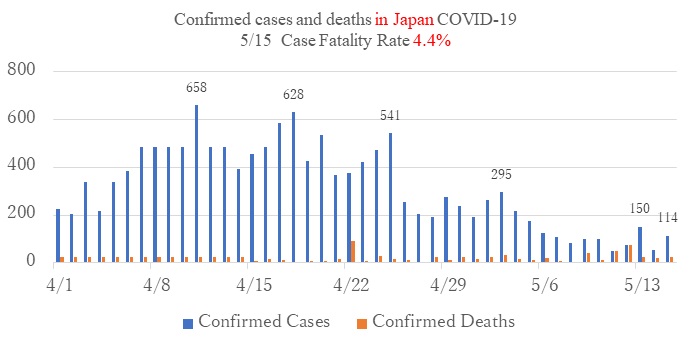
- The number of daily confirmed cases is decreasing nationwide as well as in the Tokyo metropolitan area.
- On May 14th, the Japanese government lifed the state of emergency in 37 prefectures, also planning to include 8 prefectures on May 22nd.
- In Tohoku, Chugoku, Shikoku, Kyusyu areas, very few new cases have been confirmed.
- In Hokkaido, Tokyo, Chiba, Kanagawa prefectures, and Hokuriku area (Nigata, Ishikawa, Toyama), the number of daily confirmed cases either increases or continues at the same rate.
- Reference:
2.Is the Japan Model effective as a strategy?
- The Japanese government's strategy to combat COVID-19 is different from that of China and some western countries who have imposed a lockdown to limit human movement forcibly.
- The number of new, confirmed cases and deaths is comparatively smaller in Japan. This strategy has been working quite well to contain the epidemic to date.
- The Japan model allows for a certain level of economic activity and maintains people's freedom to move about in their communities. This could prove to be a more sustainable measure over the long term than more burdensome models such as lockdowns.
- The cluster-based approach, which is the basis of Japan Model, had been taken to combat the Ebola endemic; identify the cluster, isolate the individuals involved, and monitor their close contacts. The cluster-based approach to combat COVID-19 is derived from a hypothesis obtained from an epidemiological study based on Chinese data. This hypothesis posits that the explosive increase in infected persons is a result of the high transmissibility of certain infected individuals, which forms a cluster. This approach was taken in Hokkaido in February 2020, and adapted as a national strategy through the present.
- Another key component to the Japan model is the social distancing method known as "the three Cs": closed spaces with poor ventilation, crowded places with many people nearby, and close-contact settings such as close-range conversations. The declaration of a state of emergency made it possible to avoid these three Cs. As a result, overcrowded conditions decreased by 70% in Ginza, Shibuya, Shinjuku, and the passenger rate decreased to 30 % thus avoiding crowded commuter trains in the Tokyo metropolitan area.
- This cluster-based approach and the three Cs measure may seem weak countermeasure to the eyes of people in countries where strict lockdowns have been adopted. However, this approach has not been practiced overnight. Trained public health nurses at local health centers are backbones of the cluster-based approach team. Those public health nurses who are familiar with their community have been working to identify the source of the cluster and blocking the route of infection.
- Enhancing the Japan model are factors such as the habit of wearing masks. This habit is widespread in Japan and without any social stigma, making the possibility of contraction by droplet comparatively small. Behavior like shaking hands, hugging and kissing, and other forms of physical contact are not part of traditional Japanese greetings.
- Japanese countermeasures have been criticized for their low testing rates. The Japan Model focuses on decreasing the fatality case through the treatment of severe cases and not the mild cases. Therefore, PCR testing is limited to patients with a possible risk of worsening. Due to time-consuming and lack of lab technicians, PCR testing still counts less than 10,000 daily testing. The Ministry of Health, Labour, and Welfare is expecting that rapid testing will soon be able to increase the total testing within the limits of time and human resources. However, increased testing is not the MHLW's priority according to their strategy. Even in western countries, the testing of mild cases has not been a priority because of a large number of patients.
・https://jeaweb.jp/covid/links/guide_0421.pdf
Koto K, RN, SHARE advisor
*****
1.Global and Japanese Situation of COVID-19
Confirmed cases of COVID-19 worldwide according to reports by WHO Update 2020/5/22 (Japan Standard Time) :
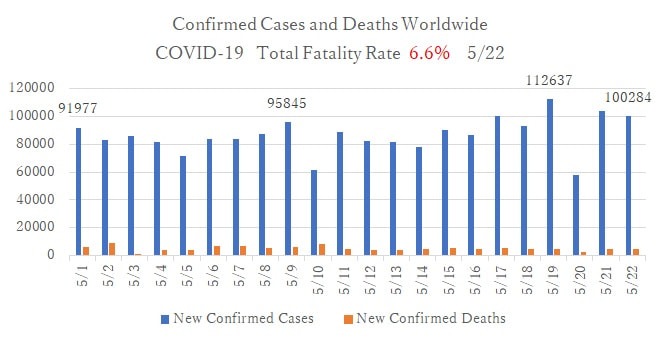
- Globally, the number of daily confirmed cases continues at more than 100,000.
- The daily confirmed cases also continue in: USA (more than 20,000); Brazil (from 10,000 to 15,000), and Russia (from 8,000 to 9,000). In Europe, the daily number of confirmed cases is decreasing.
Tokyo 2020/5/22(Japan Standard Time): MOHLW, Japan
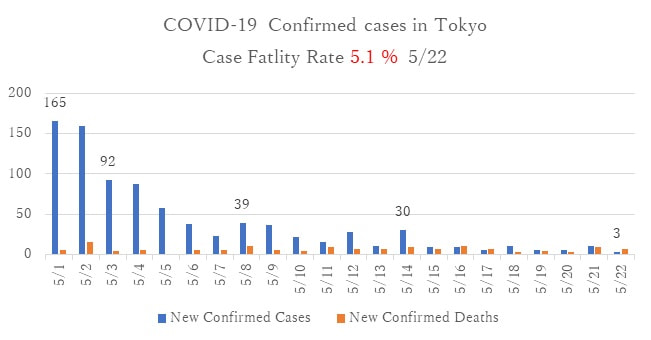
- The number of daily confirmed cases is decreasing nationwide as well as in the Tokyo metropolitan area.
2.Why the number of death cases in Japan is smaller than other countries? The care for senior citizen at elder care homes.
- Care homes across Europe and the USA came into the spotlight over COVID-19 death rate, even though care homes are generally well prepared. Coronavirus clusters occurred in these residential care homes that did not provide added or supervised medical health care. Death rates in these residential care institutions have been significantly higher than in the general population. For instance, deaths in care homes account for almost half of all deaths in Sweden, one-third in France, and one-fifth in the United States.
- One of the factors that has facilitated the lower death rate among Japanese elderly is that elderly care has been provided in the hospital, and the number of residential care homes in Japan is relatively small. The nursing care bed rate per 1,000 population is 33.6 in Japan, 53.5 in France, and 71.5 in Sweden. Hospitals, here in Japan have 30% of these care beds, while in France it is less than 10%, and less than 5% in Sweden. Although Japan is a super-aging society, it can be said that hospitals are more responsible for elderly care. Additionally, older patients could stay at the hospital as long as they wished due to the low self-payment for eldercare.
- Another facilitating factor in Japan to be considered is that medical experts advised caregivers regarding infection control. The Ministry of Health, Labour and Welfare promotes the coordination between medical care and eldercare. For example, there are full-time medical doctors at long-term care facilities (Kaigo Rojin Hoken Shisetsu [1] ), visiting medical doctors at special elderly nursing home (Tokubetsu Yogo Rojin Home [2] ) and at other types of residential care homes.
- Sweden, has been critiqued because the government discouraged care home workers from sending residents into hospitals, as well as prevented care home and nursing staff from administering oxygen without a doctor's approval.
- Korea, where they are also experiencing a rapidly aging population, refers to the Japanese medical and elderly care insurance system and has increased nursing care beds by 36% in the last decade. 60% of these nursing care beds are in hospitals, which is the highest rate globally. The Korean government has successfully controlled the outbreak and has a smaller fatality rate related to COVID-19
[1] :Provides rehabilitation and care for the elderly who aims to live at home.
[2] :Provides care for the elderly who wish to stay throughout their lives.
Reference:
・https://diamond.jp/articles/-/236988?page=2
・https://www.bbc.com/news/world-europe-52704836
・https://www.theguardian.com/world/2020/apr/09/care-homes-across-globe-in-spotlight-over-covid-19-death-rates
・https://www.nytimes.com/2020/04/17/us/coronavirus-nursing-homes.html
3.High COVID-19 attack rate following exposure at choir practice
- CDC reported that superspreading events caused COVID-19 at Skagit county, Washington, on March 17th.
- According to CDC, "Following a 2.5-hour choir practice attended by 61 persons, including a symptomatic index patient, 32 confirmed and 20 probable secondary COVID-19 cases occurred; three patients were hospitalized, and two died. Transmission was likely facilitated by close proximity (within 6 feet) during practice and augmented by the act of singing. The potential for superspreader events underscores the importance of physical distancing, including maintaining at least 6 feet between persons, avoiding group gatherings and crowded places, and wearing cloth face coverings in public settings where other social distancing measures are difficult to maintain during this pandemic."
- Adding to the above events, the pandemic on cruise ships and clusters at live houses explains the importance of avoiding the 3Cs (closed spaces, crowded places, and close-contact settings).
Reference:
- ・High SARS-CoV-2 Attack Rate Following Exposure at a Choir Practice -- Skagit County, Washington, March 2020
- ・Weekly / May 15, 2020 / 69(19);606-610
・https://www.cdc.gov/mmwr/volumes/69/wr/mm6919e6.htm?s_cid=mm6919e6_e&deliveryName=USCDC_921-DM28272
Koto K, RN, SHARE advisor
*****
1.Global and Japanese Situation of COVID-19
Confirmed cases of COVID-19 worldwide according to reports by WHO Update 2020/5/29 (Japan Standard Time) :
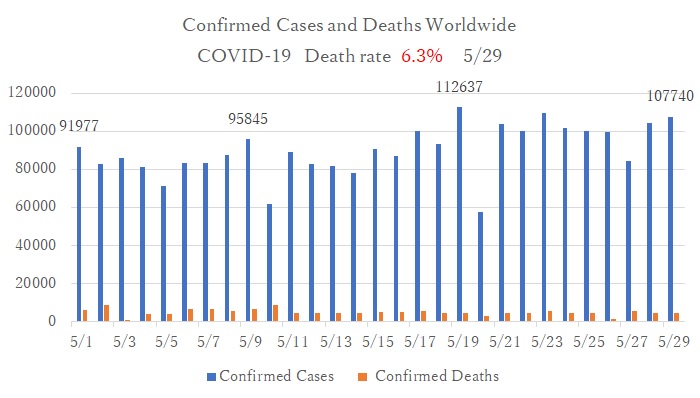
- Globally, the number of daily confirmed cases is increasing. The pandemic continues in Russia, Brazil, and India. The number of daily confirmed cases is increasing in South Asian countries such as Pakistan and Bangladesh; South America, the Mediterranean, and middle eastern countries, such as Saudi Arabia and Quate. Infection among migrant workers in the middle east accounts for most of the cases.
- In Europe, while the number of daily confirmed cases decreased, the governments in Europe began gradually easing lockdown restrictions. The fear now is of these actions triggering a second wave of COVID-19.
- In the Southeast Asian region, the rate of increase continues to slow down.
Tokyo Prefecture Report 5/29
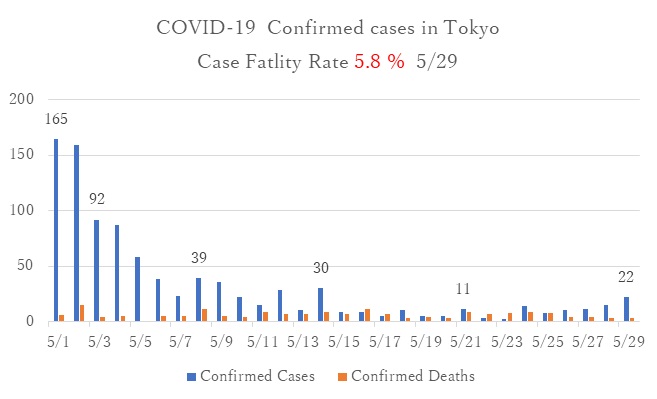
- Although the state of emergency was lifted on May 25th, the daily confirmed cases are showing a gradual increase. Clusters are developing at medical facilities in Ehime, Hokkaido, and Kitakyusyu in Fukuoka prefecture.
2.Return to work guidelines for patients with mild confirmed or suspected cases
- Mild confirmed cases that are diagnosed by a responsible medical facility or public health center, and 14 days after starting isolation and/or quarantine at designated facilities or homes. If the patients are determined to be able to return to normal daily life, he or she may return to work.
- Mild suspected cases (e.g., the person who had a fever or flu symptoms, but undiagnosed with COVID19) can end self-isolation eight days after the onset of symptoms AND must experience a resolution of fever or other symptoms for at least three days without medication (Japan Society for Occupational Health).
- The workplaces need to welcome their employee who has recovered from COVID19. The employer should not require the certificate of virus-free or recovery from the disease because it is complicated to diagnose virus-free status. Also, public health centers need to focus on diagnosing newly confirmed cases rather than proving the recovery of the patients.
- Moreover, the accuracy of self-testing kits for COVID19 falls behind that of PCR testing at the lab. The physician cannot and will not be responsible for the results of self-testing kits.
- The Act on the Prevention of Infectious Diseases and Medical Care for Patients with Infectious Diseases stipulates for patients to refrain from working. Some employers who provide social welfare services (e.g., nursery, care home) may want to announce their employee's status of virus-free for their client's comfort. However, they should be aware that "anyone could be infected," and "anyone can infect without noticing." Therefore, the employer must restrict suspected cases from their work, and encourage them to rest at home. This is proper infection control in workplaces.
Reference:
・https://note.stopcovid19.jp/n/n74204fb1d5f1
・https://note.stopcovid19.jp/n/nbc124bd1d18b#qsZJf
・https://www.mhlw.go.jp/content/000618525.pdf
・https://www.sanei.or.jp/images/contents/416/COVID-19guide0511koukai.pdf
・https://www.ecdc.europa.eu/sites/default/files/documents/covid-19-guidance-discharge-and-ending-isolation-first%20update.pdf
3.Who are eligible to receive coronavirus economic response package?
- On April 20th, coronavirus economic response package was approved by the cabinet decision.
- Foreign residents who are listed on the country's Basic Resident Registration as of April 27th are eligible to receive the 100,000 yen as part of its coronavirus economic response package.
- Basic Resident Registration is based on possessing a residence certificate with name, date of birth, sex, and address. If foreign residents with a residence card move into town, they must register into the designated municipality.
- Among foreign residents who are not listed on the country's Basic Resident Registration as of April 27th, if they were not able to return to their home country (e.g., former trainee, former students), or are the children of those who are applying for refugee status, they are eligible to receive this economic response package. Those who hold short stay status or status with designated activities for a three-month shall apply for the status with designated activities for six-months and need to register in Basic Resident Registration (as of May 19th).
- Foreign people who stay for a short term for sightseeing or business, those who overstay in Japan without visiting visa, are not eligible to receive this package.
- The municipality where you are registered will send an application form to the head of every registered household. The head of the household has to fill out their name, date of birth, address, and bank account number, and application bank account, and send the applications back with copies of their ID and bank account information.
- The link below explains how to fill out the application form in multiple languages.
http://www.ne.jp/asahi/rink/rink/index.html - Those have a My Number Card (Individual Number Card) can apply on the website.
Reference:
・https://kyufukin.soumu.go.jp/en/
・https://www3.nhk.or.jp/nhkworld/en/news/backstories/1057/
・https://migrants.jp/news/office/20200520.html
Koto K, RN, SHARE advisor
*****
1.Global and Japanese Situation of COVID-19
Confirmed cases of COVID-19 worldwide according to reports by WHO Update 8/24/2020 (Japan Standard Time) :
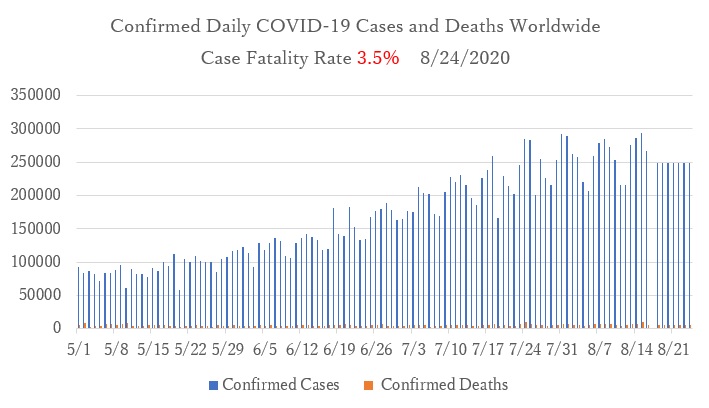
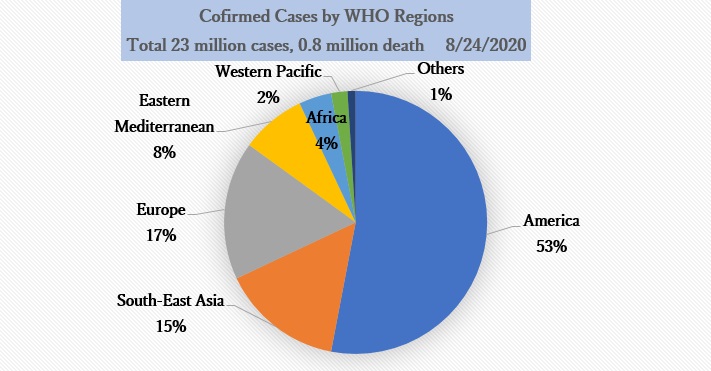
The number of daily new cases worldwide, which had been on the rise following the explosion of infections in the Americas, India and South Africa, peaked in mid-August 2020 and is following a downward trend. The cumulative number of positive cases totaled 23 million and there are more than 800,000 total dealths. The regional distribution of positive cases is as follows: the United States, Brazil and other regions of the Americas (54.5%); Southwest Asia, India and other regions of Southwest Asia (15.2%); Europe, where many countries have experienced outbreaks (17.2%); South Africa and other parts of Africa (8.8%); the Middle East, where medium-sized infections continue to occur (4.4%); Western Pacific region, where holding off the increase of infection (2.2%). The fatality rate among positive cases decreased from 6.9% in April to 3.5% in August.
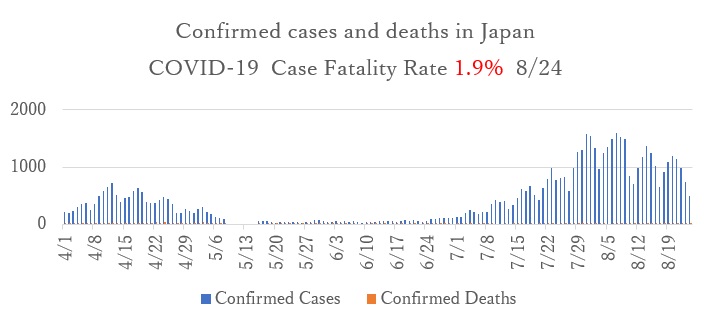
The number of daily new cases in Japan was decreasing after the state of emergency had been declared in April and May. However, in July the spread of infection in Tokyo and other urban areas began again. Infections then increased nationwide, resulting in a so-called second wave of infection. The epidemic again peaked in late July/early August and has declined since late August. The trend in the number of daily positive cases in Tokyo is similar to that in Japan as a whole. 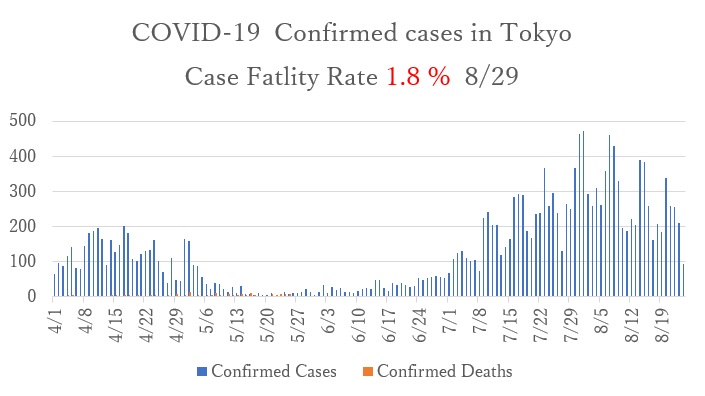
2.The Future of the COVID-19 Epidemic in Japan
In Japan, the public mostly complied with the policy of voluntary curfews following the declaration of the state of emergency in April. As a result, the nationwide curfew was successful and infections were temporarily under control. The second wave of outbreaks began in July in response to the "Go To Campaign", a governmental measure to stimulate consumption to support industries that have suffered a sharp decline in sales due to COVID-19 restrictions, such as tourism and entertainment. The second wave has been better controlled due to preventive measures taken by each municipality. However the epidemic is expected to continue in the future. The reasons for this are as follows:
- According to the results of antibody tests conducted by the Ministry of Health, Labour and Welfare (MHLW) in June on 7,950 people, only a small number of residents had been infected with COVID-19 (0.10% in Tokyo, 0.17% in Osaka, and 0.03% in Miyagi Prefecture), therefore most people do not have immunity to the virus. Exposure to SARS-CoV-2 in places like the 3Cs (Closed spaces, Crowded spaces, Close-contact settings) is highly likely to result in viral transmission. With the current expansion of economic activity and inevitable contact between people, the risk of infection from asymptomatic or mildly ill individuals is unavoidable. Also, as a result of contact outside of the household, infection may occur in one's household without members being aware of it.
- It is difficult for the government to take any further policy measures at the expense of the economic stability. Even if there is an outbreak in the future, as long as the medical supply system is in place to deal with infections, it is unlikely that another state of emergency will be declared, like in April. The country is expected to adopt policies for economic recovery.
- In the world, in countries where the number of positive cases has increased by more than 1,000 due to previous outbreaks of community-acquired infections (e.g., Iran, European countries, Indonesia), the epidemic has not ended and the number of positive cases has remained above 500-1000 for more than four months. Japan is also expected to continue to have a daily number of about 500-1000 positive cases.
- In order to contain the COVID-19 epidemic, effective vaccines, which are being developed around the world, must be administered to the population. It is expected that it will take at least two years to develop a vaccine without significant side-effects and produce enough of it to inoculate the world population.
3.Exemption from COVID-19 Inspection Fees in Japan by Installing the COCOA application
- The COCOA Contact Confirmation App is a smartphone application that allows users to receive notifications about possible contact with a COVID-19 infected person. It is a tool that uses the proximity communication function (Bluetooth) of a smartphone, with the consent of the user, to deliver notifications about possible contact with a COVID-19 positive person.. By using a smartphone's Bluetooth, contact is confirmed without either party knowing each other so that their privacy is ensured.
- On August 21, the Ministry of Health, Labour and Welfare (MHLW) indicated that COCOA users who have been notified by the MHLW that they may have been in contact with a COVID-19-positive person will also be subject to administrative testing and will not be asked to bear the cost of the testing (i.e., will be paid by the government).
- If a patient's health status deteriorates within 2 weeks of their test, the patient is required to report it immediately via COCOA. That time the patient should be promptly retested.
- It should be noted that the test cannot be used to prove the patient is virus negative.
https://gemmed.ghc-j.com/?p=35627
https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/cocoa_00138.html
4.Support Available to Foreign Residents of Japan
1)Special Cash Payment Plan
- Foreign nationals whose names were recorded in the Basic Resident Register as of April 27, the reference date, will be eligible for these benefits.
- On May 19 it was announced that (former) technical intern trainees and (former) foreign students who have difficulty returning to their home countries, as well as children of refugee claimants, would also be eligible for the special cash payment plan. Technical intern trainees and international students with "Temporary Visitor" or "Designated Activities (three months)" status will need to apply for permission to change their status of residence to "Designated Activities (six months)" and register their status with the Basic Resident Register.
- The application deadline has passed in most local governments, but in some cases, it has not yet been closed.
- Applicants can apply by filling in their bank account information on the application form mailed by the municipality to the recipient. The form must be mailed back to the municipality together with documents confirming the bank account and copies of personal identification documents. Alternatively, holders of a "My Number Card" (individual number cards for social security and tax number system) can apply electronically by entering the payee account on "Myna Portal" (government online service site) and uploading the appropriate confirmation documents for the payee account.
https://migrants.jp/news/office/20200520.html(Ijyuuren: Solidarity Network with Migrants Japan)
https://kyufukin.soumu.go.jp/ja-JP/cities/application_deadline.html (Application deadlines for each municipality)
2)Temporary Special Benefit for Households with Children
- Households that are registered with the Basic Resident Register and receive a child allowance (households with children aged 0 to junior high school students) will be paid 10,000 yen per eligible child. No application is required and the allowance is paid automatically.
- A family who has a "Student" visa holder and has (an) eligible child/children who have a "Dependent" visa status is also eligible to receive the benefit.
https://www8.cao.go.jp/shoushi/shinseido/taiou_coronavirus.html
3)Temporary Loan Emergency Funds(mainly for households with income shortage)
- A maximum of 200,000 yen will be loaned to households that are affected by COVID-19 restrictions, have experienced a decrease in income due to absence from work, etc., and require emergency and temporary living expenses to maintain their lives.
https://www.tcsw.tvac.or.jp/
Dr. Aya Yumino
*****
1.Global and Japanese Situation of COVID-19
■Confirmed cases and new deaths from COVID-19 worldwide(source: WHO, updated 2020/9/28)
Case fatality rate: 3.1%
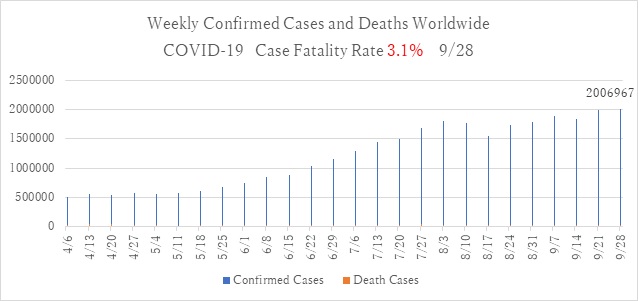
- There is a total of 32.63 million positive cases and more than 990,000 deaths worldwide, with a case fatality rate of 3.1%. (WHO, updated 2020/9/28)
- Globally, the rate of increase for the number of new positive cases by week has remained unchanged, and the maximum peak of the increase has passed.
- In the African and Western Pacific regions, the number of cases has begun to decrease. In the European region and the Eastern Mediterranean region, the epidemic has re-emerged in September after a temporary downward trend. The number of cases in these locations is higher than in April. In the European region, France and Spain had numbers of new cases (more than 5,000 cases per day) confirmed to be larger than that during April-May. This increase can be considered as a second wave of outbreak of infection.
- In the US region, infection continues to spread.
- In the Southwest Asia region, the number of new positive cases is increasing due to an explosion of infections in India, which currently has the largest number of cases in the world, while the number of new positive cases is decreasing in other Southwest countries.
- In Southeast Asia and the Western Pacific, there have been no outbreaks reported in Thailand, Vietnam, Laos and Cambodia.
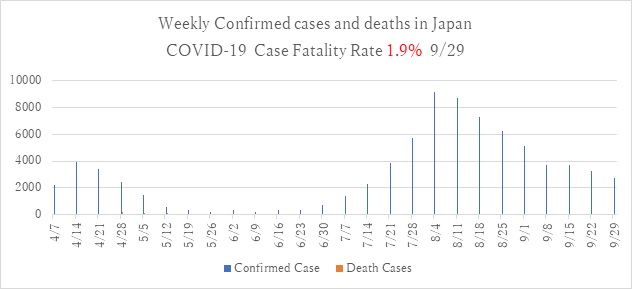
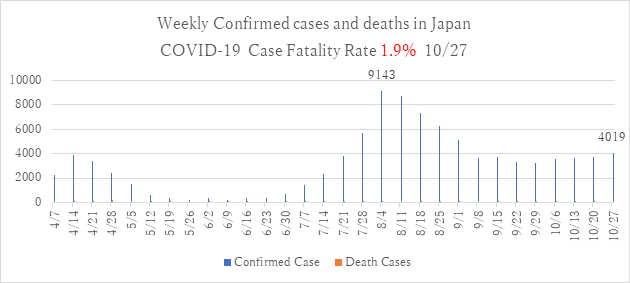
■Weekly confirmed cases and deaths of COVID-19 in Japan (updated 2020/9/28)
- Case fatality rate 1.9%
■Weekly confirmed cases of COVID-19 in Tokyo (updated 2020/9/29)
- Case fatality rate 1.7%
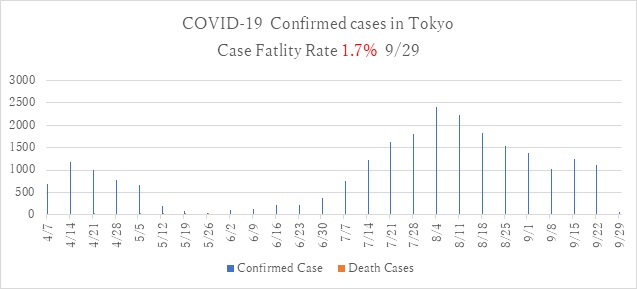
- In Japan, the number of new positive cases from late July to early August has been decreasing, and the overall trend is downward in the metropolitan Tokyo area and other areas. It can be said that the second wave of infection is over.
- As of September 28, fewer than 100 new cases per day have been reported in Tokyo, and more than 10 positive cases have been reported in Hokkaido, Ibaraki, Saitama, Chiba, Kanagawa, Osaka, Hyogo, Kyoto, Hiroshima, and Okinawa, although these numbers are following a decreasing trend.
- Infection is under control in the Tohoku, Hokuriku, Shikoku, and Kyushu regions.
2.Accelerating Vaccine Development, Many Questions Remain
- Vaccination is one of the most promising measures against new corona virus infections. Effective and safe vaccination may prevent serious illness and death due to infection. In addition, as with yellow fever, mandatory vaccination would allow people to return to the same international migration behavior as before the COVID-19 epidemic. This would restore the movement of people between nations, and would also provide the countries opportunities for economic recovery.
- The development of vaccines by pharmaceutical companies in Europe, the U.S., and China is progressing, and it is reported that vaccines will be approved in the near future.
- Many questions have been raised in the midst of overheated news reports on the vaccine. The first is the timing of vaccine approval. Normally, vaccine development is a time-consuming process. In the past, even the fastest approval had taken four years. However the urgent need for the vaccine has spurred development, and drug companies are spending huge amount of money to ensure that clinical trials can proceed quickly, and there are six vaccines that have begun clinical trials. The U.S. Food and Drug Administration (FDA) says any vaccine must have at least a 50 percent chance of preventing disease, which is the same effectiveness as a regular Influenza vaccine. Not all vaccine candidates will succeed to pass this standard, and there is a risk that money and manpower will be wasted on vaccines that fail.
- Another issue is fair vaccine distribution. After the vaccine is ready, the first nations in line to get it are the high-income countries that have supported the vaccine's development, such as the US and the UK. There is currently no global body to guarantee fair distribution.
- There is the possibility that all the vaccines may have side effects and that they can only provide immunity for a short period of time.
- It is worrying that governments around the world have put pressure on regulators to approve vaccines that have not been proved to be effective. On August 11st, Russia approved one vaccine before even conducting the final phase of trials that would normally be performed to prove the effectiveness of the vaccine. An ineffective vaccine even can increase the risk of larger spread of the target disease by allowing people to let them down the guard of those who receive it.
- The ultimate goal of mass vaccination is the acquisition of herd immunity. This means that a sufficient number of people must gain immunity in order to make it harder for the infection to spread. Vaccinating 70% of the population would require a large amount of funding, so this goal may not be feasible.
- Expectations for a new vaccine against the new coronavirus are high in Japan as well, but even if it is successfully developed, it is not yet known how effective the vaccine will be.
- ・
Column: Accelerating Vaccine Development, Many Questions Remain
- ・
Widespread anxiety over corona vaccine, world says 'I won't get vaccinated'
- ・
Vaccine 'not to be overly hopeful'... effectiveness unknown, concerns over side effects
3.What will change under the new Japanese government's policy against COVID-19?
- On August 28, the Japanese government's task force came up with a new policy to deal with COVID-19, including a review of the testing system.
- In the past, the main route for testing was to contact consultation centers set up by public health centers and undergo testing at specialized outpatient clinics or community outpatient/testing centers set up by local medical associations, etc. In addition to this, the new plan is to test for Influenza and SARS-CoV-2 be done simultaneously at local clinics to strengthen the testing system.
- The hospitalization procedures for people with COVID-19 will also be reviewed. Specifically, those who are asymptomatic or mildly ill will not be hospitalized at medical institutions, but will be given thorough treatment at lodging facilities or at home in principle. Even up until now people with no symptoms were, in principle, required to stay at home or lodging facilities. However, there were many cases in which they were required to be hospitalized, depending on the region in which they were confirmed to be positive. The aim of this review is to reduce the number of people to be hospitalized, so that limited medical resources can be focused on the treatment of seriously ill patients and reduce the burden on local health centers that arrange patient hospitalization.
- The Ministry of Health, Labor and Welfare (MHLW) is extending the period of the "employment adjustment subsidy" from the end of September to the end of December, which started as a measure to protect employment stability. Since February this year, MHLW has been offering these special measures to companies affected by COVID-19. The maximum subsidy has been increased from 8,330 yen to 15,000 yen per person per day. The rate of subsidies for other payments such as absence allowance for employees has been increased to 75% for large companies and 100% for small and medium-sized companies.
- The Japanese government plans to downgrade COVID-19 from its current category of infectious diseases. Infectious diseases are classified as Category 1-5, with COVID-19 being classified as "Category 2 or equivalent" at present. Category 2 infectious diseases are currently identified as those needing measures such as admitting seriously ill people to hospital and advising asymptomatic people to be hospitalized, in order to isolate those who tested as positive. Under the new policy, the recommendation to admit asymptomatic and mildly ill patients is to be removed in order to ensure that beds are available for the critically ill. At present, the mildly ill are required, in principle, to be kept in isolation in an accommodation facility, but this measure will no longer be mandatory. In addition, it is likely that the accommodation for those asymptomatic and mildly ill will no longer be fully funded by the public and will require payment from those accommodated.
- ・
What will change under the new Japanese government's policy against COVID-19?
- ・
We need to be careful about revising the rules for COVID-19 countermeasures
- ・
Corona "Class 2 removal" amidst the mess over Prime Minister's resignation
Dr. Aya Yumino
*****
1. Global and Japanese Situation regarding COVID-19
■Confirmed cases and new deaths from COVID-19 worldwide(source: WHO, updated 2020/10/19)
Case fatality rate:2.8%
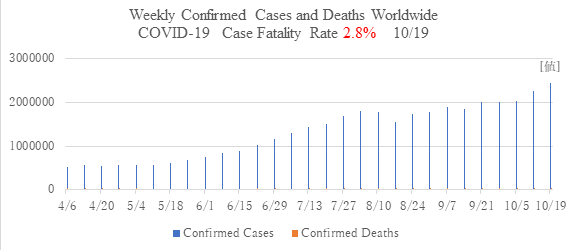
- There are more than 40 million total positive cases of COVID-19 and more than 1,100,000 deaths worldwide, with a case fatality rate of 2.8%. (WHO, updated 2020/10/19)
- Globally, the number of new weekly positive cases is rising again, reflecting a sharp increase in Europe. Meanwhile, the fatality rate is on the decline.
- In the Eastern Mediterranean, African and Western Pacific regions, the trend of new cases is also shifting from decreasing to increasing, albeit gradually.
- In the Americas and Southwest Asia, where the number of new cases is increasing rapidly in India, the number of new cases is larger than in the rest of the world. But the number has peaked and is now on a downward trend. These two regions account for half of the world's positive cases.
- The European region saw three times as many new infections and deaths in October as in April. France, the United Kingdom, Russia, the Czech Republic and Italy all currently have an explosion of infections.
- India, the United States, France, Brazil and the United Kingdom were the countries with the highest number of new cases in the last week of October. Weekly confirmed cases and deaths of COVID-19 in Japan (updated 2020/10/27)
-Case fatality rate 1.9%
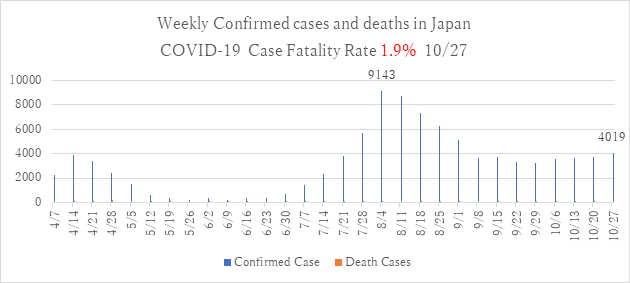
■Weekly confirmed cases and deaths of COVID-19 in Japan (updated 2020/10/27)
- Case fatality rate 1.9%
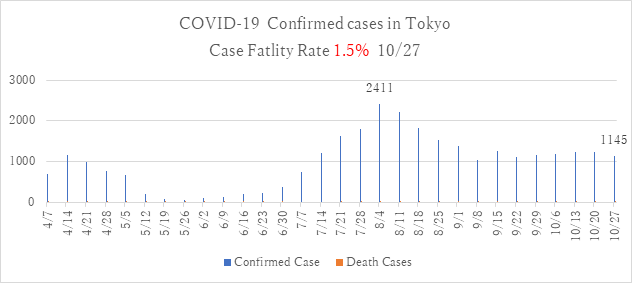
■Weekly confirmed cases of COVID-19 in Tokyo(updated 2020/10/27)
- Case fatality rate 1.5%
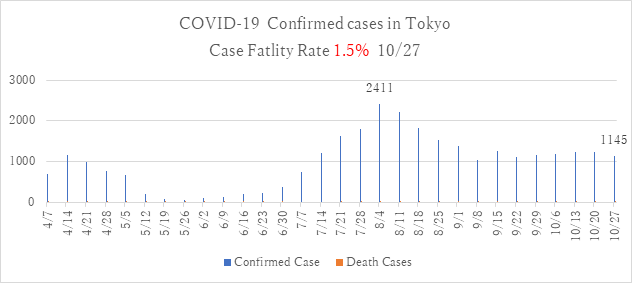
- The downward trend of new positive cases has leveled off in the Tokyo metropolitan area and nationwide, with 500 new cases reported for Japan as a whole and 150-200 new cases in Tokyo each day. This trend is expected to continue.
- New positive cases in the Tokyo metropolitan area and in cities such as Miyagi, Osaka, Hyogo, and Fukuoka continue to be reported.
- In October, the number of new cases increased in Kumamoto, Okinawa, and Hokkaido, which had a particularly marked increase.
- In the Hokuriku, Shikoku and Kyushu regions infections are under control.
2. Drastic Strengthening of Border Measures at Ports and Airports
Ministry of Health, Labour and Welfare (updated 2020/10/06)
- All persons entering Japan must stay at a place designated by the quarantine station chief (e.g., home) for 14 days after arrival, use a means of non-public transportation from their arrival point to their place of stay, and register their place of stay and the means of transportation with the quarantine station.
- Those who have stayed in areas subject to refusal of entry to Japan (many countries are subject to this rule) are required to undergo a test for SARS-CoV-2 at the time of entry, to wait in a space at the airport or in a facility designated by the quarantine station until the results of the test are available. They must stay in a secured area for 14 days from the date of entry, even if the results of the test are negative, and will be subject to health verification by a health center during the stay.
- If their test result is positive, the person will be quarantined in a designated institution such as medical facilities, hotels and home.
- Those who departed from an area subject to denial of entry to Japan within the last 14 days and arrived via a different country are also subject to the border measure, but if Japan is only a transit point and they do not enter the country, they are not subject to the measure.
- For 14 days from the day of arrival, travelers must stay at the place designated by the quarantine center chief (such as home, accommodation owned by company, relative's house, friend's house, apartment rented by month, or hotel booked by independently) and they may not go out.
- If you stay at home, it is important to wash your hands frequently, get enough sleep, and take care of your nutrition. If symptoms such as cough or fever occur, you should call the Consultation Center for the Returnees and the appropriate contact persons in advance of visit, and go to the designated medical facility.
- Families and others who must spend time in close proximity with the newly arrived person during the quarantine should try to reduce contact as much as possible, wash their hands frequently, wear masks and limit the number of people they come into contact with if they feel unwell.
- The health center monitoring each arrival will check the health status of the arrived person daily by phone or email for 14 days after arrival in Japan.
- https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/kenkou_iryou/covid19_qa_kanrenkigyou_00001.html#Q3-2 (Japanese)
- https://www.mhlw.go.jp/stf/covid-19/kansenkakudaiboushi-iryouteikyou_00005.html (English)
*****
1. Global and Japanese Situation regarding COVID-19
■Confirmed cases and new deaths from COVID-19 worldwide(source: WHO, updated 2020/10/19)
Case fatality rate:2.8%
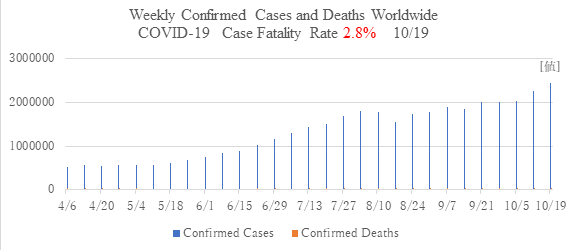
- There are more than 40 million total positive cases of COVID-19 and more than 1,100,000 deaths worldwide, with a case fatality rate of 2.8%. (WHO, updated 2020/10/19)
- Globally, the number of new weekly positive cases is rising again, reflecting a sharp increase in Europe. Meanwhile, the fatality rate is on the decline.
- In the Eastern Mediterranean, African and Western Pacific regions, the trend of new cases is also shifting from decreasing to increasing, albeit gradually.
- In the Americas and Southwest Asia, where the number of new cases is increasing rapidly in India, the number of new cases is larger than in the rest of the world. But the number has peaked and is now on a downward trend. These two regions account for half of the world's positive cases.
- The European region saw three times as many new infections and deaths in October as in April. France, the United Kingdom, Russia, the Czech Republic and Italy all currently have an explosion of infections.
- India, the United States, France, Brazil and the United Kingdom were the countries with the highest number of new cases in the last week of October. Weekly confirmed cases and deaths of COVID-19 in Japan (updated 2020/10/27)
-Case fatality rate 1.9%
■Weekly confirmed cases and deaths of COVID-19 in Japan (updated 2020/10/27)
- Case fatality rate 1.9%
■Weekly confirmed cases of COVID-19 in Tokyo(updated 2020/10/27)
- Case fatality rate 1.5%
- The downward trend of new positive cases has leveled off in the Tokyo metropolitan area and nationwide, with 500 new cases reported for Japan as a whole and 150-200 new cases in Tokyo each day. This trend is expected to continue.
- New positive cases in the Tokyo metropolitan area and in cities such as Miyagi, Osaka, Hyogo, and Fukuoka continue to be reported.
- In October, the number of new cases increased in Kumamoto, Okinawa, and Hokkaido, which had a particularly marked increase.
- In the Hokuriku, Shikoku and Kyushu regions infections are under control.
2. Drastic Strengthening of Border Measures at Ports and Airports
Ministry of Health, Labour and Welfare (updated 2020/10/06)
- All persons entering Japan must stay at a place designated by the quarantine station chief (e.g., home) for 14 days after arrival, use a means of non-public transportation from their arrival point to their place of stay, and register their place of stay and the means of transportation with the quarantine station.
- Those who have stayed in areas subject to refusal of entry to Japan (many countries are subject to this rule) are required to undergo a test for SARS-CoV-2 at the time of entry, to wait in a space at the airport or in a facility designated by the quarantine station until the results of the test are available. They must stay in a secured area for 14 days from the date of entry, even if the results of the test are negative, and will be subject to health verification by a health center during the stay.
- If their test result is positive, the person will be quarantined in a designated institution such as medical facilities, hotels and home.
- Those who departed from an area subject to denial of entry to Japan within the last 14 days and arrived via a different country are also subject to the border measure, but if Japan is only a transit point and they do not enter the country, they are not subject to the measure.
- For 14 days from the day of arrival, travelers must stay at the place designated by the quarantine center chief (such as home, accommodation owned by company, relative's house, friend's house, apartment rented by month, or hotel booked by independently) and they may not go out.
- If you stay at home, it is important to wash your hands frequently, get enough sleep, and take care of your nutrition. If symptoms such as cough or fever occur, you should call the Consultation Center for the Returnees and the appropriate contact persons in advance of visit, and go to the designated medical facility.
- Families and others who must spend time in close proximity with the newly arrived person during the quarantine should try to reduce contact as much as possible, wash their hands frequently, wear masks and limit the number of people they come into contact with if they feel unwell.
- The health center monitoring each arrival will check the health status of the arrived person daily by phone or email for 14 days after arrival in Japan.
- https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/kenkou_iryou/covid19_qa_kanrenkigyou_00001.html#Q3-2 (Japanese)
- https://www.mhlw.go.jp/stf/covid-19/kansenkakudaiboushi-iryouteikyou_00005.html (English)
*****
1. Global and Japanese Situation regarding COVID-19
■Confirmed cases and new deaths from COVID-19 worldwide(source: WHO, updated 2020/11/29)
Case fatality rate:2.4%
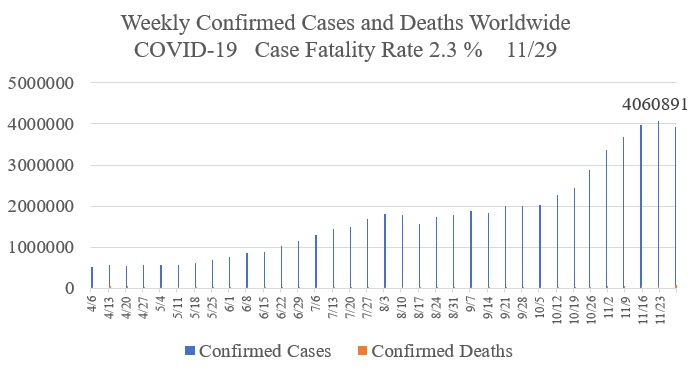
- Worldwide, the number of new positive cases every day is about 4 million, and there are more than 53.7 million total positive cases and 1.3 million total deaths, with a fatality rate of 2.4%. (WHO, updated 2020/11/22)
- Globally, the number of new positive cases per week has increased in Europe and the Americas, which accounts for 80% of new cases. While the rate of increase is high and growing in the Americas, there has been a decrease in the rate of increase in the European region due to the strengthening of public health measures.
- In the Eastern Mediterranean, African and Western Pacific regions, there is an increasing trend of the number of new cases.
- In the Southwest Asia region, including India, one of the endemic countries, the number of cases is on the decline.
- The numbers of new cases for select countries during the week of November 9-15 were: In the Americas, 1 million in the United States and 180,000 in Brazil; in Europe, 240,000 in Italy and 200,000 in France; in Southwest Asia, 300,000 in India; in the Mediterranean, 76,000 in Iran, 36,000 in Jordan, and 36,000 in Morocco; in Africa, 13,000 in South Africa; and in the Western Pacific region, 13,000 in the Philippines. The outbreak of COVID-19 in the United States stands out.
- The WHO held an extraordinary general meeting from November 9 to 14 to discuss future efforts for the countermeasures against COVID-19.
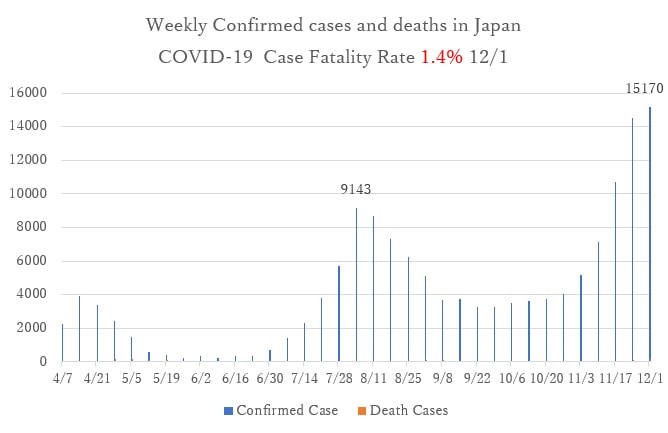
■Weekly confirmed cases and deaths of COVID-19 in Japan (updated 2020/12/1)
- Case fatality rate 1.4%
■Weekly confirmed cases of COVID-19 in Tokyo(updated 2020/12/1)
- Case fatality rate 1.2%
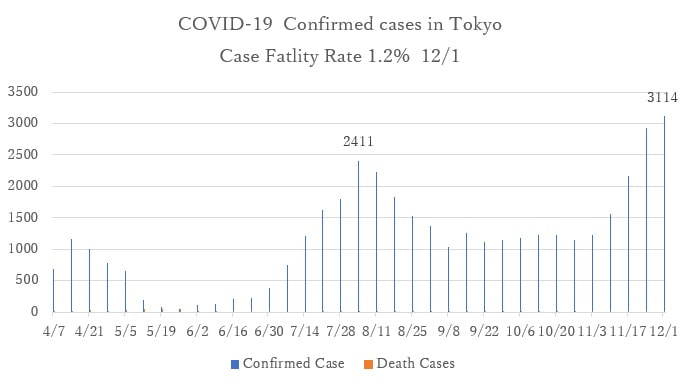
- The number of new positive cases has increased since late October. While an increase in the Tokyo metropolitan area has been seen, the number of new cases also has increased in Hokkaido, Osaka, and Aichi, leading to a nationwide increase in COVID-19 infection. The third wave of epidemic is observed.
- The places which have clusters of cases that cause the spread of the COVID-19 in the community have diversified, including dining places, workplaces, foreign resident communities, medical institutions, and welfare facilities, in addition to the orthodox cluster places such as entertainment areas of local cities. The likely causes of the outbreaks are the increase of domestic migration of people using the Go To Travel and Go To Eat campaigns and the tourism activities during the fall holiday season.
- The number of positive cases of foreigners detected at airport quarantine is also increasing. The possibility that the outbreak among foreign resident communities in Japan may be due to the infection from newly arrived members in the communities cannot be ruled out.
2. Two Effective COVID-19 Vaccines
U.S. Pfizer Inc.
- On November 20, Pfizer Inc. from the US and BioNTech from Germany announced that they have submitted a request to the U.S. Food and Drug Adminisitation (FDA) for an Emergency Use Authorization (EUA) of their COVID-19 vaccine candidate.
- Pfizer Inc. announced earlier this week that the final analysis of clinical trial data showed that the vaccine is effective in preventing new coronavirus (SARS-CoV-2) infections with a 95 percent chance of success. The company said It is effective across all age groups of adults and ethnicities, and there have been no serious safety issues so far in the trial involving about 44,000 people.
- Pfizer and BioNTech say they have applied for emergency approval not only in the U.S., but also in Australia, Canada, Europe, Japan and the U.K., which could pave the way for the vaccine to be used in "high-risk populations" by the end of December 2020.
- One challenge is that the vaccine is made from mRNA and must be stored at temperatures below -70 degrees Celsius. Amesh Adarjah, a researcher at Johns Hopkins University said "The cold chain is going to be one of the biggest challenges to vaccinating people with the COVID-19 vaccine, even hospitals in large cities don't have such ultra-cold storage facilities."
U.S. Moderna Inc.
- On November 16, the U.S. biotechnology company Moderna announced that its COVID-19 vaccine "mRNA-1273" showed 94.5% efficacy in the first interim analysis of the Phase III trial of the vaccine done by Data Safety Monitoring Committee.
- Approximately 30,000 people were divided into two groups and administered two doses of vaccine or placebo. To date, 95 people have been infected with SARS-CoV-2, of which 90 received a placebo-control and 5 received a vaccine. From this result, it was concluded that the vaccine prevented 85 people from becoming infected as compared to 90 without the vaccine, and that the vaccine was effective in 85/90 x 100 = 94.5% of the cases. Of the 95 infected patients, 11 became severely ill, but all were in the placebo-control group, so the vaccine is expected to prevent severe disease as well.
- Since mRNA is a highly unstable molecule, one of the weaknesses of mRNA vaccines is that they require ultra-low temperature refrigeration for transport and storage. However, Moderna's mRNA vaccine has special modifications and is effective for one week in regular refrigeration and six months in normal freezing (minus 20 degrees Celsius), according to the an the company.
・https://www.bloomberg.co.jp/news/articles/2020-11-21/QK4PIPDWRGG201
・https://www.bloomberg.com/news/articles/2020-11-20/pfizer-covid-19-vaccine-first-to-seek-emergency-u-s-clearance(English)
・https://jp.techcrunch.com/2020/11/23/2020-11-20-pfizer-and-biontech-to-submit-request-for-emergency-use-approval-of-their-covid-19-vaccine-today/
・https://answers.ten-navi.com/pharmanews/19723/
・https://investors.modernatx.com/news-releases/news-release-details/modernas-covid-19-vaccine-candidate-meets-its-primary-efficacy
・https://www.covid19-yamanaka.com/cont3/21.html
3. COVID-19 infections among asymptomatic persons
- ith COVID-19 infections, the responding to asymptomatic persons who can transmit the disease through breathing alone becomes a challenge.
- For example, a patient was "fine" on Saturday night and interacted with a large group of people, but on Monday he/she had a cough, fever, and fatigue and realized that he/she had been infected. The Centers for Disease Control and Prevention (CDC) estimates that people who pass the virus before they develop such symptoms account for about half of all cases of infection.
- The CDC says that asymptomatic cases account for as much as 40% of all cases in the U.S.
- It is more difficult to grasp the cases of people who are infected with the virus but show no symptoms at all. According to the CDC, as many as 40 percent of cases in the U.S. are asymptomatic.
- Why are there so many people who infect others before they develop the disease (pre-symptomatic) or without any symptoms (asymptomatic)? The viruses of influenza and common colds also can spread without symptoms. However, COVID-19 infections are extremely more difficult to detect and therefore more difficult to control.
- One of the problems is that the manifestations of the disease are not well understood. It is known that the elderly, people with pre-existing conditions such as obesity, asthma, and diabetes, are more likely to become seriously ill. However, it is not well known about those who are infected but avoid severe condition of COVID-19.
- The New England Journal of Medicine (NEJM) published the largest ever study of asymptomatic SARS-CoV-2 transmission among 1,848 U.S. Marine Corps recruits, ages 18 to 31 years old.
- The results of this study, in which nearly 2,000 young people were tested for SARS-CoV-2 showed that almost all COVID-19 infections were missed during observation for symptoms of infection. In the study, it was suggested that a wide range of routine testing of asymptomatic as well as symptomatic individuals is needed to control the spread of infection.
・https://news.yahoo.co.jp/articles/c342abf8d9387caf7e77b7eeaa13984c524c371a
・SARS-CoV-2 Transmission among Marine Recruits during Quarantine
・https://www.nejm.org/doi/full/10.1056/NEJMoa2029717?query=TOC
・https://jp.wsj.com/articles/SB11922503875527593554104587093463746193648
*****
1. Global and Japanese Situation regarding COVID-19
■Confirmed cases and new deaths from COVID-19 worldwide(source: WHO, updated 2020/12/13)
Case fatality rate:2.3%
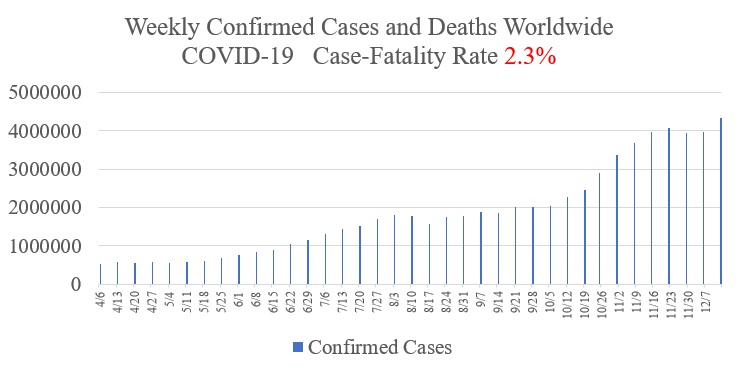
- With approximately 4.3 million new positive cases and over 75,000 new deaths per week worldwide, the COVID-19 epidemic is growing. The case-fatality rate is 2.3%. The total number of positive cases has exceeded 70 million and the number of deaths has reached 1.6 million. (WHO, updated 2020/12/13)
- The four countries that have reported the most cases worldwide in the past month are the U.S., Brazil, India, and Russia. The U.S. is experiencing a particularly high rate of increase, with more than 200,000 new positive cases being identified every day.
- In the African region, the epidemic is coming back, with notable increases of COVID-19 cases in Mali, Nambia, Nigeria, Senegal, and South Africa.
- In the Eastern Mediterranean and European regions, the number of cases is on a downward trend.
- The Southwest Asia region has seen a downward trend in the number of cases as the rate of increase in india, the largest endemic country in the region, has decreased.
- In the Western Pacific region, the number of cases is on the rise, especially in Japan, although its share in the global cases is small.
■Weekly confirmed cases and deaths of COVID-19 in Japan (Updated 2020/12/8)
- Case fatality rate 1.5%
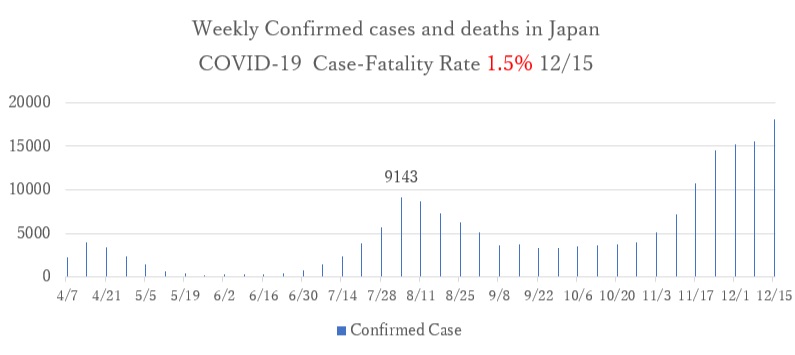
■Weekly confirmed cases of COVID-19 in Tokyo (Updated 2020/12/8)
- Case fatality rate 1.2%
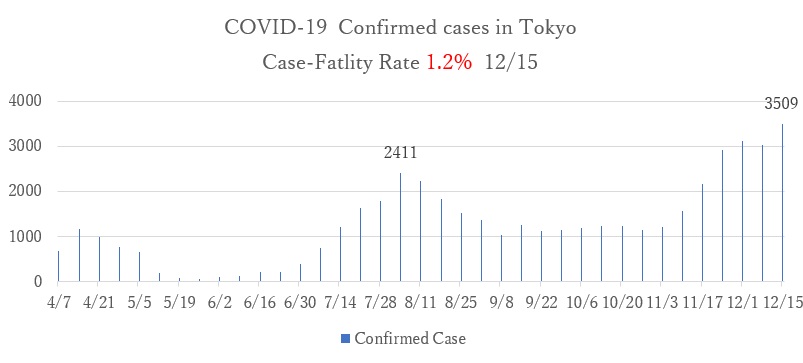
- The number of new positive cases in Tokyo is reaching 300-500 daily, suggesting that the epidemic is continuing. There is an increasing trend in the Tokyo metropolitan area, Aichi Prefecture, Osaka, Kyoto, Hyogo, Fukuoka, and other large regional cities, suggesting that the epidemic is continuing nationwide.
2. Vaccination and Immunity
- It was reported that patients infected and symptomatic with SARS-CoV-2 may remain immune to the virus for at least six months afterwards. This suggests that the effect of vaccination lasts as long as natural immunity.
- On the other hand, Imperial College London, a British university, announced the results of a study that showed even after people recover after being infected, their antibodies rapidly decrease within three months. "Herd immunity," the ability to contain the infection by allowing most of the population to become infected, recover and build immunity, may not be possible with this virus.
- Vaccination is expected to prevent COVID-19, however it is necessary to ensure the safety of vaccination. If the rate of side effects is high or there are serious adverse events like death, the vaccine is not suitable for public use.
- With multiple vaccines being developed (six deployed in humans as of December 15, including from the U.S., U.K., China, and Russia) simultaneously, there is a good chance that a vaccine will be found that suits each individual.
- The UK's Medicines and Healthcare products Regulatory Agency (MHRA) has announced that people who have had anaphylactic reactions to medicines or foods should not be vaccinated with the Pfizer COVID-19 vaccine.
- On December 13, clinical trials of a vaccine developed by Sinopharm, a major Chinese pharmaceutical company, were temporarily suspended in Peru because one subject showed neurological symptoms.
・"Immunity to COVID-19 may persist six months or more: Evidence is emerging that the coronavirus sparks potentially lasting protection in some people"
・"An mRNA Vaccine against SARS-CoV-2 -- Preliminary Report"
・"Is the fast-developed COVID-19 vaccine more dangerous than the virus?"
・"COVID-19 Vaccine Adverse Reactions to be Reviewed by Each Country: WHO Peru cancels clinical trial of Chinese-made vaccine for neurological symptoms."
3. Characteristics of COVID-19 patients
This is a summary of the symptoms, course, and severity of COVID-19 that have been raging around the world in 2020. We now know about the after effects, which were not known in the early stages of the pandemic.
- The incubation period for the virus ranges from 1 to 14 days, and most people develop the disease in about 4 to 5 days. Symptoms are similar to those of colds and influenza, including cough, shortness of breath, difficulty breathing, fever, chills, muscle pain, joint pain, vomiting, diarrhea, and abnormal sense of smell and taste. In particular, shortness of breath, olfactory and taste disturbance are rare symptoms in colds and influenza, which may trigger suspicion of coronavirus infection.
- Symptoms such as fever and cough accompany olfactory and taste disturbances increase the likelihood of COVID-19, although similar conditions can also be seen with colds, sinusitis, and hay fever.
- According to data from 40,000 infected people in China during the early stage of the epidemic, the initial onset of the disease is followed by minor symptoms like a cold for about a week, and about 80% of the people recover without any symptoms, but less than 20% become seriously ill.
- From the data collected in Japan since June, elderly people and patients with chronic illnesses are most likely to become seriously ill from COVID-19. The rate of people who become seriously ill is about 1.6% (0.3% in those under 50 and 8.5% in those of 60 and over), and the mortality rate is about 1.0% (0.06% in those under 50 and 5.7% in those of 60 and over). The severity of the disease is reportedly higher in males than in females.
- It has been reported that about 30-40% of people infected with COVID-19, especially young people, are asymptomatic. For example, in a cluster of young people on the U.S. nuclear-powered aircraft carrier USS Theodore Roosevelt, 1,271 of the 4,779 crew members tested positive by PCR, of which 45% were asymptomatic at the time of testing, 32% were asymptomatic and later developed symptoms, and 23% were symptomatic.
- The most infectious period is considered to be from two days before to seven to ten days after the onset of the disease. Viral shedding is thought to be particularly high just before and after disease onset.
- The severity of the disease has been found to vary depending on a patient's pre-existing conditions. In the U.S., the risk of hospitalization is 1.5 times higher for asthma, 3 times for hypertension, 3 times for obesity (BMI >30), 3 times for diabetes, 4 times for chronic kidney disease, 4.5 times for severe obesity (BMI >40), 4.5 times for two underlying diseases, and 5 times for infected individuals with three or more comorbidities.
- In Japan, 10-20% of patients continue to have sequelae such as cough, phlegm, lethargy, dyspnea, olfactory disturbance, and taste disorder as long as 60 days after onset of the disease, and 2-11% have these sequelae 120 days after initial onset.
- In France, hair loss, memory impairment, sleep disturbance and poor concentration, have been reported as sequelae.
・"Symptoms, course and risk of severe COVID-19, and guidelines for seeking medical attention"
・Ministry of Health, Labour and Welfare, "10 Knowledge Points on the Present State of COVID-19"
*****
1. Global and Japanese Situation regarding COVID-19
■Confirmed cases and new deaths due to COVID-19 worldwide(source: WHO, updated 2021/1/24)
Case fatality rate: 2.2%
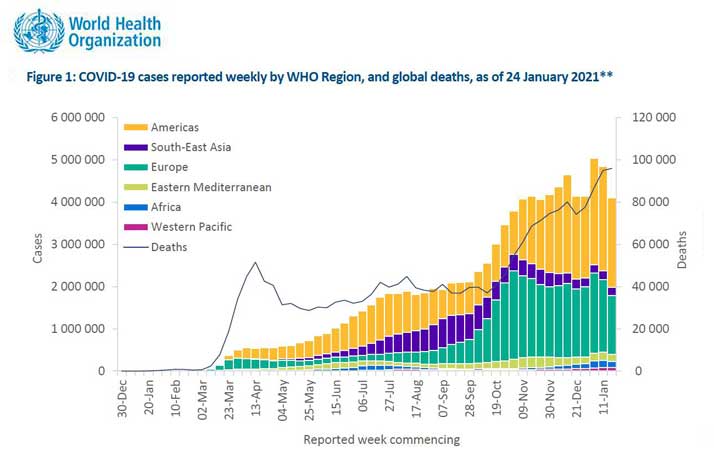
To cite fromWHO(World Health Orgbanization) :weekly-epidemiological-update---27-january-2021
With approximately 4-5 million new positive cases and over 85,000 new deaths per week worldwide, the COVID-19 epidemic seems to have reached the upper limit of the rate of case increase. The case fatality rate is 2.2%. The total number of positive cases has reached almost 100 million, and the number of deaths has exceeded 2.1 million. (WHO, updated 2021/1/24)
The status of the case increase in the third week of January:
- The five countries with the highest number of reported cases worldwide are the United States, Brazil, the United Kingdom, Russia, and France. The U.S. continuing to experience the highest rate of increase, with more than 200,000 new cases being confirmed every day.
- The number of new positive cases in the Americas region is high, especially in the U.S., Brazil, and Colombia.
- In the third week of January, the Africa region saw the notable increases in South Africa, Nigeria, and Zambia.
- In the Asian region, increases are seen in Japan, Malaysia, the Philippines, and Indonesia. In India, although the absolute number is large, there is a downward trend.
■Weekly confirmed cases and deaths due to COVID-19 in Japan
Case fatality rate 1.4% (updated 2021/1/26)
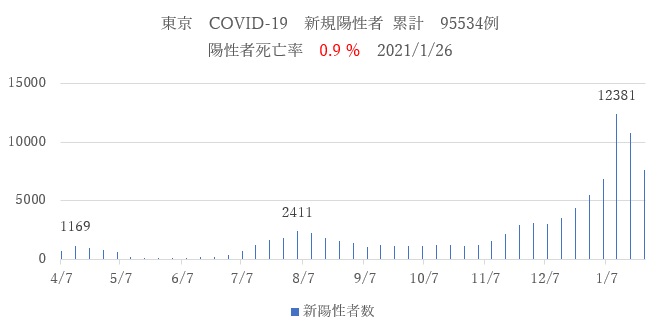
■ Weekly confirmed cases of COVID-19 in Tokyo
Case fatality rate 0.9% (updated 2021/1/26)
- The number of new positive cases in Japan and Tokyo is thought to have increased sharply in the first and second weeks of January due to people's movement and outings during the Christmas and New Year holidays. A state of emergency has been declared in the Greater Tokyo area from January 8 (Tokyo, Chiba, Saitama, and Kanagawa), and in other seven prefectures from January 14 (Tochigi, Gifu, Aichi, Kyoto, Osaka, Hyogo, and Fukuoka). Since the third week of January, the number of new positive cases has been on a downward trend both in Tokyo and nationwide.
2. SARS-CoV-2 Mutant Strains
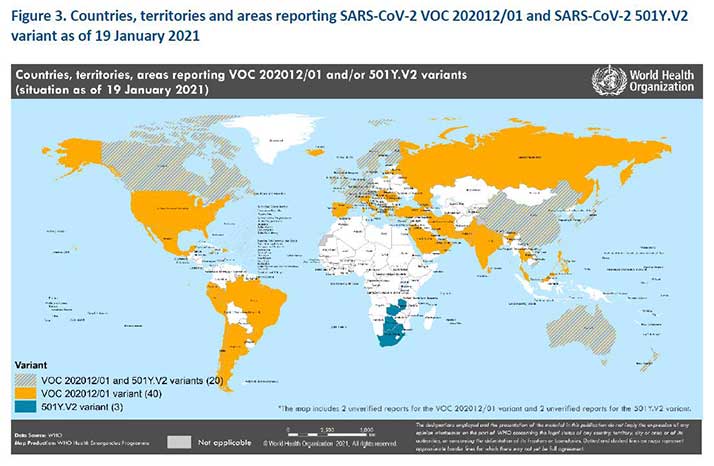
To cite fromWHO(World Health Orgbanization):weekly-epidemiological-update---19-january-2021
- Currently, several COVID-19 mutant strains are prevalent around the world.
- The new variant, called B.1.1.7 (VOC 202012/01), which emerged in the United Kingdom (UK) and has been reported in 60 countries as of January 19. The variant is observed to spread more easily and rapidly than other variants, but there is no evidence that it causes more serious illness or increased risk of death.
- In South Africa, a variant strain called 1.351 (501Y.V2) has emerged. It was originally detected in early October and has been reported in 23 countries as of January 19.
- A variant called P.1 appeared in Brazil and was detected in four travelers to Japan.
・https://www.who.int/publications/m/item/weekly-epidemiological-update---19-january-2021
・https://www.cdc.gov/coronavirus/2019-ncov/transmission/variant.html
3.Household Transmission
- The results of 54 related studies showed that the household infection rate of COVID-19 in 77,758 people was 16.6%, which was higher than those of SARS (7.5%) and MERS (4.7%). The household infection rate among symptomatic patients was 18.8%, which was higher than that of asymptomatic patients (0.7%). In total, 28.3% of the transmissions were through contact with adults, while 16.8% were through contact with children. The infection rate from spouses (37.8%) was higher than that from other family members (17.8%). The household infection rate tended to be higher when the number of people living together was small: 41.5% for those living with one other person and 22.8% for those living together with three or more people.
- Household Transmission of SARS-CoV-2 A Systematic Review and Meta-analysis
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2774102
4. Ten Facts about the "Now" of COVID-19
(Ministry of Health, Labour and Welfare: MOHLW; January 2020)
- In Japan, about 209,980 people have been diagnosed with COVID-19, which is equivalent to about 0.3% of the total population.(2021/1/29)
- 2. The proportion of people diagnosed with novel coronavirus infections who become severely ill or die depends on their age, and tends to be higher among the elderly and lower among the young.
・1.6% of patients become seriously ill (0.3% in under 50 and 8.5% in 60 and above).
・1.0% of patients die (0.06% for those under 50 and 5.7% for 60 and above).
- The elderly and those with underlying diseases (chronic obstructive pulmonary disease (COPD), chronic kidney disease, diabetes, hypertension, cardiovascular disease, and obesity) are more likely to develop serious symptoms. Pregnant women and those with a history of smoking are also considered to be more susceptible to infection.
- The number of infections and deaths per population in Japan has remained low compared to the global average and major countries.
- The period in which a person infected with the new coronavirus may infect others is considered to be from two days before symptom onset to seven to ten days after onset. It is also reported that within this period, viral shedding is particularly high immediately before and after the onset of illness.
- The risk of infection increases in three-C environments (Closed spaces, Crowded places and Close-contact settings), because SARS-CoV-2 is mainly transmitted through droplet and contact infections. It is also important to note that infection can easily occur in situations such as social gatherings with drinking, eating and drinking in large groups or for long periods of time, conversations without masks, living together in a small space, and switching places to stay.
- It has been observed that less than 20% of people diagnosed with new coronavirus infections also infected others, and over 80% have not infected others. Therefore, if an infected person takes infection prevention measures in three-C environments which will limit contacts and thus viral spread, the COVID-19 pandemic can be controlled.
- Tests for diagnosing novel coronavirus infection include PCR tests, antigen quantitative tests and qualitative tests, all of which are used to detect the presence of the virus in a person's body. With the development of new testing methods, it is now possible to use saliva or nasal swabs in addition to nasopharyngeal swabs, depending on the patient's condition and testing environment. The antibody test is designed to determine whether a person has had COVID-19 in the past, so it cannot be used to diagnose an infection at the time of the test.
- Mild cases often resolve spontaneously and symptomatic treatment such as antipyretics are given when necessary. In cases of respiratory failure, oxygen administration, steroids (anti-inflammatory drugs), and antiviral drugs may be administered, and if there is no improvement, intensive care with a ventilator or other equipment may be used. However, the elderly and those with underlying medical conditions should be aware that their condition may suddenly worsen.
- COVID-19 vaccines are being vigorously researched and developed overseas and in Japan. In some countries, emergency use of vaccines has been approved and vaccination has started. An application for approval of the vaccine has been filed in Japan, and the approval review is underway based on the results of clinical trials in Japan and overseas. Preparations are being made to ensure that those who wish to receive the vaccine will be able to do so as soon as the review is completed and approved. In general, vaccines are effective in preventing the onset and aggravation of infectious diseases. Researchers collaborating with Pfizer, Moderna, and AstraZeneca have published the interim results from a Phase III trial showed that fewer people who received the vaccine developed COVID-19 than those who did not. In general, while extremely rare, adverse reactions to vaccinations are possible. Adverse reactions to COVID-19 vaccines have been confirmed in clinical trials and ongoing other studies.
*****
Benefits of vaccination
- There are two pillars: prevention and treatment to fight against COVID-19. In order to prevent infection, it is necessary to disinfect the environment and wash our hands thoroughly to avoid contact infection. We must wear a mask to reduce contact with the virus from infected people and avoid contact with many people in the "Three C environments" (closed spaces, crowded places, and close-contact settings). The most fundamental way of preventing infection is for our bodies to produce antibodies that will fight against the virus through immunization (vaccination). Vaccination prevents the new coronavirus from increasing in the body and preventing the onset of COVID-19. Vaccination can also prevent the progression of virus-related illness leading to a serious condition and death.
- Generally, when many people are infected with the disease, "herd immunity" will be achieved and the epidemic will subside. However, in the case of COVID-19, herd immunity is difficult to achieve because the antibodies produced in the body of an infected person last only about six months.
Vaccine approval
- Since April 2020, more than 70 different vaccines have been developed and tested in clinical trials.
- On February 12, 2021, the Japanese Ministry of Health, Labour and Welfare (MHLW) gave fast-track approval to Pfizer's COVID-19 vaccine for manufacture and distribution, after confirming its efficacy and safety through data from clinical trials. The approval in Japan comes two months later than in Europe and the United States. Pfizer's vaccine is administered to people aged 16 and over in two doses, three weeks apart. After vaccinating selected doctors and nurses, the plan is to inoculate about 3.7 million other healthcare providers in March and start vaccinating about 36 million elderly people in April. AstraZeneca, a British company, applied for approval to manufacture and distribute their COVID-19 vaccine in Japan on Feb. 5, and the government has also decided to receive supplies from the U.S. company, Moderna.
Adverse events of the vaccines
- In general, adverse health effects to vaccinations are unavoidable, although they are extremely rare. The overseas vaccines that are planned to be supplied to Japan (vaccines being developed by Pfizer, AstraZeneca, Moderna and Novavax) are not currently considered to have raised any serious safety concerns. On the other hand, there have been reports of adverse events after vaccination, including those not causally related to vaccination, such as pain at the site of the vaccination, headache, fatigue and myalgia. Anaphylaxis (acute allergic reaction) was also reported to have occurred in rare cases in vaccinations already carried out overseas. If anaphylaxis occurs, it should be treated immediately at the location where the vaccination was administered, or at a medical institution.
Vaccine recipients
- In principle, vaccine recipients of the new coronavirus vaccine should be vaccinated in the municipality where their residence is located, as each region will establish its own vaccination system for its residents. On the other hand, if a person is unable to receive a vaccination ticket from their municipality due to unavoidable circumstances, the municipality will issue a vaccination ticket and administer the vaccination if the actual status of the person's residence is recognized. Homeless people and foreigners living in Japan who do not have a residence certificate may be eligible.
■Reference:
Nikkei News: Suga says Japan's vaccinations to begin in the middle of next week
-Country set to start inoculation with Pfizer jabs, starting with health workers
(Japanese) (English)
Ministry of Health, Labour and Welfare (MHLW):10 things to know about the COVID-19 as of right now(As of January 2021)
*****

नेपाली भाषा ネパール語情報
Tiếng Việt ベトナム語情報
မြန်မာ ミヤンマー語情報
■Useful URLs by multi-languages
- 【Information for foreign residents(A)】
- 【Information for foreign residents(B)】
- 【Information for foreign residents(C)】
Donation すべての人と健康を
シェアする活動を、
毎月の寄付で
応援しませんか?
シェアは、いのちを守る人を育てる活動として、保健医療支援活動を現在
東ティモール・カンボジア・日本の3カ国で展開しています。
- 寄付で応援する(support/donation/index.html)
寄付で応援する
マンスリーサポーター、
一回のみの寄付、
遺贈による寄付などが可能です。 - モノを集めて、 モノを購入して支援(support/mono.html)
物の寄付で応援する
書き損じハガキ、未使用の
はがきや切手、商品券、使用済みの
切手による寄付が可能です。 - ボランティア・インターンとして参加(support/volunteer/index.html)
参加して応援する
スタッフ、ボランティア・
インターンとしてシェアに
参加することが可能です。